By Dr. Sarah Bennett, NMD / February 6, 2020
There is a chance that you’ve heard about how incredibly important your thyroid is for a number of functions… but why is that?
It’s been a minute since high school biology class, so you’re not alone in scratching your head and trying to remember what the thyroid does. That said, it is crucial in so many ways, so there is no time like the present to learn!
So, without further ado, what is the thyroid? Why is it so important? Here is everything you need to know in a quick ultimate guide! (Below is a video for you visual learners)
The thyroid is a butterfly-shaped endocrine gland located at the base of the neck. Its main responsibility is to secrete hormones that regulate your metabolism and serum calcium levels.
Usually, discussions about thyroid functionality are referring to its regulation of metabolism rather than calcium. So, for now, this is what I will stick to. By extension, these conversations also typically refer to the hormones that regulate your metabolism (triiodothyronine (T3) and thyroxine (T4)).
To dive in a little deeper, we’re going to go over the thyroid hormones and their function. This will help to give a more in-depth understanding of how important it is to your body and its everyday needs.
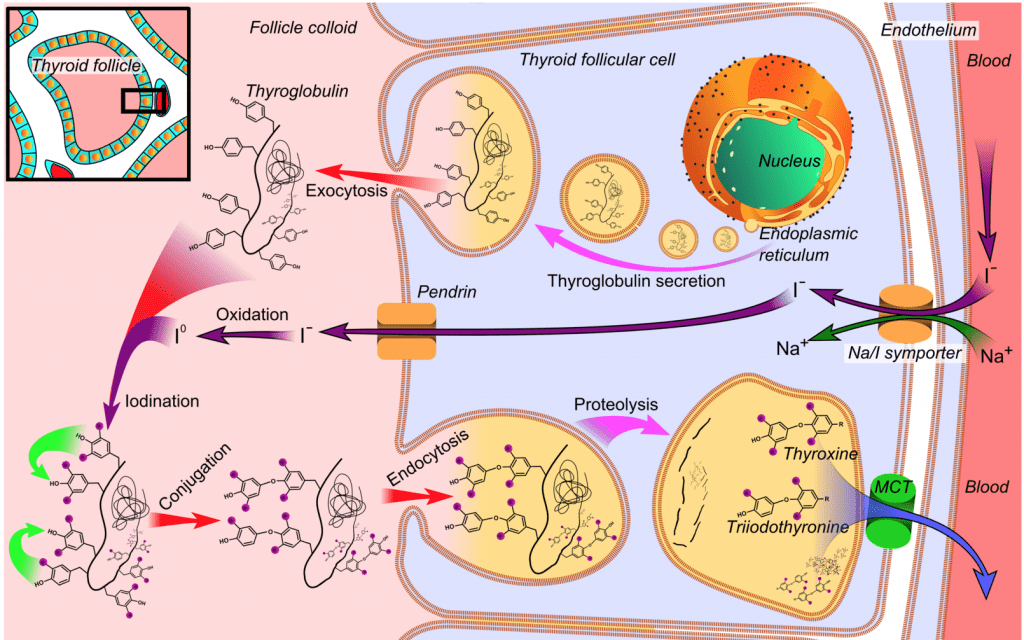
Thyroid hormones are created in the thyroglobulin of the colloid. Thyroidperoxidase enzymes will join tyrosine and iodine molecules to form DIT (diiodotyrosine) and MIT (monoiodotyrosine) which are precursors to thyroid hormones.
When TSH (thyroid-stimulating hormone) stimulates the thyroid, the tyrosine molecule is cleaved and T4, T3, and some RT3 are bound and released into the bloodstream. T4 and T3 are released from the thyroid in an 80% to 20% ratio with the vast majority of these hormones bound to thyroid-binding globulin. Thyroid-binding globulin is a protein-carrier designed to transport these hormones to the rest of your body.
While T4 is the most abundant thyroid hormone in circulation, it is primarily inactive until converted to T3. T4 acts primarily as a prohormone to T3, the most biologically active thyroid hormone. Once transported to the periphery, T4 is converted to T3. In times of high stress, injury, and illness, T4 may also be converted to RT3.
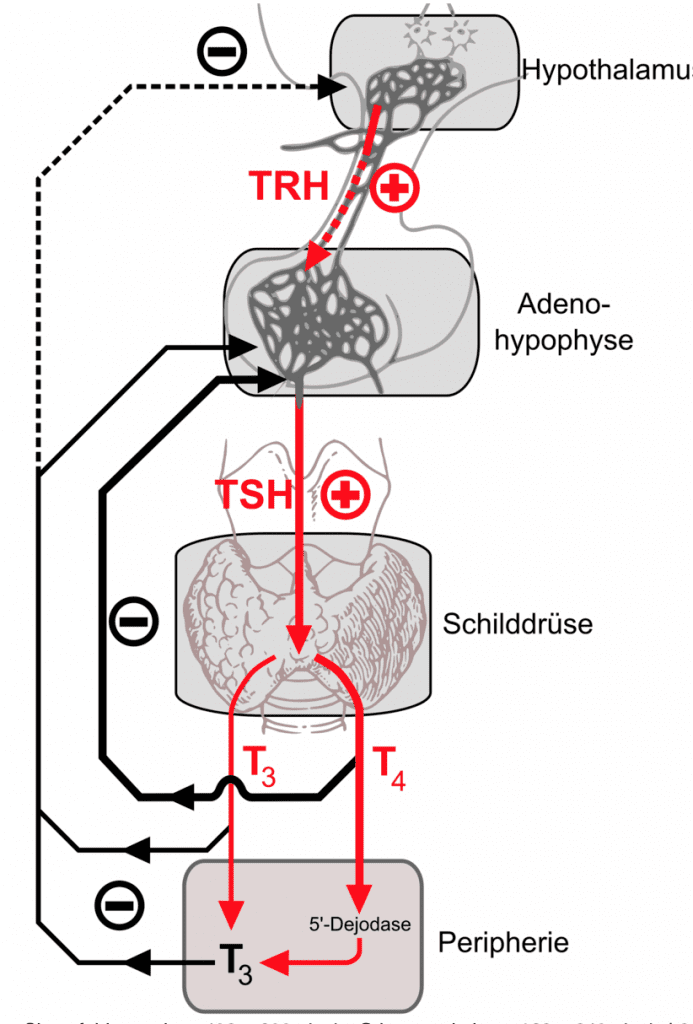
So… how does the body regulate your thyroid hormones? In a healthy body, the Hypothalamus, Pituitary, Thyroid (HPT) axis will keep these hormones tightly regulated. When thyroid hormone levels are low, the hypothalamus releases Thyroid Releasing Hormone (TRH) which travels through the bloodstream to the pituitary gland to stimulate the release of TSH.
Then, TSH proceeds to travel through the bloodstream to the thyroid gland to stimulate the release of T3 and T4. When thyroid hormones reach a level that satisfies the brain set point, the production of TRH and TSH will stop, creating a negative feedback loop. T4 will primarily signal the pituitary gland to discontinue production of TSH while T3 will signal the hypothalamus and pituitary to discontinue production of TRH and TSH respectively.
To better understand this and additional terminology used in this article, we are going to highlight the main protein, enzyme, and hormone testing that we do at Natural Med Doc to ensure optimal levels:
Thyroid-stimulating hormone (TSH) is the most frequently run thyroid marker. It is oftentimes used as the sole measure of thyroid function. The higher this number, the louder the brain is speaking when asking for more hormones.
Ultimately, we want a low number around 1.00 to indicate a satisfied brain. Although many providers may use this as their one and only marker for thyroid, I have found that it is insufficient at best. I often see that even with an optimal value for TSH that T3 and T4 are not within optimal limits. This means that your brain perceives suboptimal T3 and T4 levels as sufficient.
I have also seen TSH values significantly out of range while T3 and T4 levels are not mirroring the problem. This is often indicative of other disease processes.
I refer to triiodothyronine (T3) as your engine fuel. This is because it is the most biologically active thyroid hormone.
Free T3 is more commonly tested than Total T3 because the bound T3 is not what activates the tissues. Roughly 80% of T3 is bound while only 20% is free or available for the body to use.
This hormone directly impacts your metabolism, energy, mood, immune function, bowel movements, and cognitive clarity. Throughout the day, thyroxine (T4) is converted to T3 to maintain your energy. The reference range for this value may differ between each lab, but the optimal adult value for T3 lies between 3.2-4.8 pg/ml.
I find that my patients feel their best near the upper end of this range. Most reference ranges use 2.0 pg/ml as the lower limit. My lower limit is 3.2 pg/ml based on the fact that research has shown improved cardiovascular health when above this range.
Even if your lab values do not diagnose you with hypothyroidism, you may experience the same or similar symptoms if your thyroid hormones are simply suboptimal, also knowing as subclinical hypothyroidism. This is why you should always test and care for these levels under the supervision of a naturopathic physician.
T4 is the most abundant thyroid hormone in the body. It acts as a prohormone to T3. Deiodinase enzymes will convert T4 to T3 in the periphery.
75% of T4 in the body is bound to the thyroid-binding globulin, making it inactive (much like with T3). This means that T4 is mostly inactive overall. This is why testing Free T4 is more common than testing Total T4 as well.
It is important to have a healthy Free T4 to Free T3 ratio. Research has found that this ratio is important for maintaining a healthy body weight! If this ratio is off, it may indicate other pathological processes or inappropriate conversion.
Reverse T3 (RT3) is the third most common thyroid hormone. It is primarily produced from T4 converting down a different pathway in the peripheral tissues. RT3 is an isomer of your healthy T3 molecule, meaning that it competes with your healthy T3 levels to bind cellular thyroid receptors.
It is metabolically inactive, and will put your body into a hibernation state when elevated. Additionally, RT3 can contribute aggravating hypothyroid symptoms when elevated. In times of high stress, starvation, or illness, your body will naturally begin to convert T4 to RT3, increasing your levels and causing unwanted symptoms.
Thyroid peroxidase (TPO) is an enzyme in the thyroid gland that is important for the production of thyroid hormones. TPO will oxidize iodine ions in the thyroid colloid to form iodine which then attaches to the thyroglobulin to form T3 and T4.
Anti-TPO antibodies are the most common thyroid antibody and are found in over 80% of Hashimoto’s and Grave’s Disease patients. If you have been diagnosed with autoimmune thyroiditis or you are unsure if your thyroid condition is related to an autoimmune condition, this is an important marker to have checked.
It is important in thyroid management to not only resolve symptoms but to also decrease antibody levels to preserve proper thyroid function.
Thyroglobulin is the most abundant protein within the thyroid gland. It is also an important precursor to thyroid hormones. Thyroglobulin antibodies are not only found in more than 50% of Hashimoto’s and Grave’s Disease patients, but also in 25% of thyroid cancer patients. If this comes back positive, it is vital to follow up with your managing provider!
Remember, antibody levels are important to consider during thyroid management. For optimal thyroid management, decreasing antibody levels should be a priority. Why? Because elevated antibodies indicate that healthy thyroid tissue is being attacked at a high rate, and decreasing the levels of antibodies decrease or eliminate the rate of destruction, ultimately preserving thyroid function.
Now that we’ve established how a healthy thyroid and its hormones function, it’s time to dive into where things can go wrong. Believe it or not, there are a variety of different diseases associated with the thyroid that go beyond “hypothyroidism” or “hyperthyroidism” (which is where we will start).
Hypothyroidism is categorized by abnormally low activity of the thyroid gland. It is a very common problem that millions of people face each year.
Hypothyroid Symptoms:
Our thyroid production naturally declines with age, progressively lowering our metabolic rate and therefore putting us into a state of hibernation.
This generally starts around the age of 30, and sometimes sooner. During this gradual process, more and more symptoms of hypothyroidism start to peek their head out.
Long ago when we lived in tribes, this process of turning down the metabolism of the “elders” would have benefited survival. It would result in leaving more food resources for the young and fertile.
Evolution has not caught up! In modern day society, we are living longer and need our energy and cognitive ability well past 50, 60, 70 years of age. I constantly see that with age, our thyroid hormone levels fall further and further away from the optimal range, leading to subclinical or overt hypothyroidism.
Hypothyroidism can be both medically induced or congenitally induced. These are each unique concerns with their own causes and implications, so we will go into the details of them both now.
Congenital Hypothyroidism is a condition caused when a baby is born with an underdeveloped thyroid gland. If this condition is not appropriately treated, it may result in intellectual disabilities and failure to thrive.
Medically induced hypothyroidism is a little more complicated. Certain medical treatments may inadvertently induce hypothyroidism. Radioactive iodine or surgical removal of the thyroid may be indicated in uncontrolled hyperthyroidism to avoid thyroid storm. As a result, the thyroid is destroyed or removed, causing lower if not entirely eliminated natural production of thyroid hormones. This results in the necessity to balance thyroid hormones exogenously.
Certain other medications may also induce hypothyroidism by altering the healthy production of thyroid hormones.
Amiodarone, an antiarrhythmic medication, alters production of thyroid hormones at the level of the pituitary, thyroid gland, and peripheral tissue. This results in an elevation of serum Free T4 and RT3 as well as a decrease in serum Free T3. This change will place your body in a hibernation state and cause hypothyroid symptoms.
Interferon-alpha, a medication used to treat many different forms of cancer and hepatitis C, has been shown to induce what is known as interferon-induced thyroiditis. This not only causes an increased risk of thyrotoxicosis in the short-term but also chronic hypothyroidism.
Lithium, a psychiatric medication, inhibits thyroid iodine uptake, iodotyrosine coupling, and thyroid hormone secretion. It also alters thyroglobulin structure, ultimately leading to hypothryoidism.
Lastly, interleukin-2, an immunotherapy prescribed to treat kidney cancer, stimulates the production of autoantibodies towards the thyroid, ultimately leading to hypothyroidism.
During pregnancy, the body will naturally suppress immunological functions to prevent the fetus from being rejected. After birth, the immune function rebounds, elevating thyroid antibody levels. Oftentimes, susceptible women have shown to display elevated thyroid antibodies.
Thyroid function will return to normal most of the time, though about 25% of women with a history of postpartum thyroiditis will develop hypothyroidism in the next ten years.
Often used to achieve weight loss have actually been shown to decrease the rate of metabolism indefinitely. More specifically, when calorie intake is restricted, calorie output or energy expenditure is decreased by an equal amount. A key factor in this change is the decrease in production of T3, the metabolically active thyroid hormone, and increase in production of RT3, the inactive isomer of T3 that competes to decrease metabolic rate.
Hashimoto’s autoimmune thyroiditis is the most common form of hypothyroidism. This disorder displays lymphocytic infiltration and fibrotic changes caused by elevated autoantibodies and affects about 1 in 1,000 people.
Typically, it presents with hypothyroid symptoms, a non-tender goiter, and elevated TPO. It also may present with possible TG antibodies. In addition to typical hypothyroid symptoms, you may experience a feeling of fullness in the lower neck over the region of the thyroid.
Many people are not aware that Hashimoto’s may present very different in its beginning stages. The autoantibodies cause the thyroid gland to be inflamed or cause thyroiditis. This causes the stored thyroid hormone to leak out of the gland and potentially produce hyperthyroid symptoms for up to about 3 months.
After 3 months, thyroid hormone levels begin to drop due to ongoing damage to the thyroid caused by elevated autoantibodies. This is when hypothyroid symptoms present and is most commonly when people are diagnosed.
This is due to the formation of a goiter (diffusely enlarged thyroid) and will generally resolve with proper management of the disease. The following factors may increase your risk of developing Hashimoto’s disease:
The optimal thyroid panel to test for Hashimoto’s includes TSH, Free T3, Free T4, Anti-TPO, and Anti-TG. Anti-TPO and Anti-TG are positive in greater than 90% of Hashimoto’s patients. It is important that these hormone levels are checked at least once a year!
On the other end of the spectrum, hyperthyroidism refers to overactivity of the thyroid gland, a condition that leads to a rapid heartbeat and an increased rate of metabolism.
Hyperthyroid Symptoms:
Subacute thyroiditis is often triggered by a viral infection causing inflammation of the thyroid gland (thyroiditis). The inflamed thyroid gland over-produces thyroid hormones and causes hyperthyroidism until the inflammation has healed. Generally, thyroid hormone production will return to normal over time.
Grave’s Disease is the most common cause of hyperthyroidism, affecting 1 in 200 people. It typically presents with hyperthyroid symptoms, enlargement of the thyroid, thyrotoxicosis (low TSH, elevated T3, and elevated T4), and TSHR antibodies.
Patients with Grave’s Disease will often present with the majority of the hyperthyroid symptoms above and goiter. In addition to the typical hyperthyroid symptoms, 33% of patients display Grave’s ophthalmopathy (bulging of the eyes) and 15-40% display Grave’s dermopathy, a lumpy reddish thickening of the skin over the shin.
Some factors that increase the risk of Grave’s Disease include:
Much like with other autoimmune conditions, symptoms often appear suddenly after a major life stressor, injury, or illness.
Once diagnosed, uncontrolled Grave’s Disease is conventionally treated with antithyroid medication like methimazole for the first 12-18 months. This reduces and manages production of thyroid hormones.
If antithyroid medication fails to decrease levels of TSHR antibodies, patients may continue antithyroid medication and re-test in 12 months or opt for radioactive iodine therapy to destroy the overactive thyroid gland. They may also opt for thyroidectomy surgery to remove the overactive gland which is commonly recommended.
Proper management is imperative to avoid an array of adverse effects. Improper management may lead to thyroid storm, infertility, miscarriages, preterm birth, preeclampsia, heart disorders, and brittle bones.
Similar to any other autoimmune condition, lowering antibody levels is imperative for the proper management of the condition. Therefore, antibody levels should be checked frequently until well controlled.
One worry and fear that haunts any patient going through complications or concerns is the possibility of cancer.
Fortunately, when compared to other cancers, thyroid cancer is rare! So if you come across a lump on your thyroid, don’t jump straight to, “I’m dying!!” To put it in perspective, there were 52,000 cases of thyroid cancer recorded in 2019 and over 268,000 cases of breast cancer. Also, thyroid cancer has a 98.2% 5-year survival rate.
There are four general types of thyroid cancer. Here they are listed in order of severity of prognosis:
Thyroid cancers are generally asymptomatic, presenting with a quickly enlarging nodule or rapid, painful diffuse enlargement of the thyroid. The following factors increase the risk of developing thyroid cancer:
Most thyroid cancers are diagnosed during routine check-ups, so don’t feel uncomfortable asking for an ultrasound of the thyroid. The best imaging for initial detection of thyroid cancer are ultrasounds and radioiodine scans.
Ultrasounds will detect enlargement, nodules, and cysts. Radioiodine scans are able to pinpoint nodules that are likely cancerous based on how the nodules uptake the iodine in the system. This scan may be recommended for all but medullary carcinoma. For full diagnosis, fine needle aspiration is the gold standard for biopsy.
While all of these conditions have their own unique characteristics and symptoms, they are all linked through causes and risk factors since they pertain to your thyroid. The most notable causes and risk factors include:
While many of these cannot be controlled, they are important to know so that you can be proactive about your thyroid and hormonal health! This way you will be able to more effectively communicate with your naturopathic doctor and get to the route of your concerns.
Now that you are more caught up with how the thyroid works and the possible dysfunctions that can occur, we can jump into the treatment options!
Levothyroxine (Synthroid)
This is a synthetically produced T4 hormone and is the most commonly prescribed thyroid medication. This is the go-to medication for conventional treatment.
Many practitioners will use this medication as a solo treatment for full thyroid management. The rationale behind this is that T4 is the most abundant thyroid hormone and will naturally convert to T3 in peripheral tissues. If a patient has hypothyroidism (low T4), then this medicine should theoretically do the trick. However, I often see otherwise, so this isn’t the ultimate cure-all!
Liothyronine (Cytomel)
This is a synthetically produced T3 hormone. As T3 is less abundant and more biologically active, a small dose is very powerful. This may be the reason that many providers do not utilize this medication in practice. However, I find that when dosed appropriately in conjunction with levothyroxine, hypothyroid symptoms improve dramatically.
Natural Medication
Firstly, there is natural medication that can be used. Desiccated thyroid medication (Naturethroid, Armour, NPthroid) is comprised of another animal’s thyroid gland and contains a combination of both T3 and T4. I use this medication frequently in practice and consistently see wonderful results!
Guggul
Gum Guggal has been shown to increase thyroid functioning in animal studies. The ketosteroid compounds increase uptake of iodine by the thyroid gland and improve enzymatic actvitiy to improve the ratio of T3 to T4.
Cleus Forskohlii
This is an herb that has recently increased in popularity due to its ability to aid in weight loss. Cleus Forksohlii helps to increase the metabolic weight through stimulating T3 and T4 secretion while improving thyroid iodine uptake and increasing cyclic AMP.
Iodine
More than 800 million people across the world are iodine deficient. Iodine is an essential precursor to thyroid hormones, so deficiency not only causes goiters but also hypothyroidism or subclinical hypothyroidism.
Though Iodine is essential for thyroid hormone production, take caution! Supplementing with high doses should be medically guided since it must be balanced with other minerals to prevent aggravation of latent autoimmunity.
If any type of thyroid autoimmunity is a current diagnosis, be sure to check with your provider prior to beginning iodine supplementation, even in lower doses. Anywhere between 250mcg-1mg per day is considered same in non-autoimmune patients.
To improve selenium concentrations naturally, eliminate Bromide. This competes for the same receptors as Iodine. It is found in pesticides, certain medications, and solvents.
Iodine may be increased dietarily as well. High concentrations of iodine are found in seaweed, iodine-fortified table salt, fish, shrimp, and eggs.
Selenium
This is another key nutrient necessary for proper thyroid hormone production. Similar to iodine deficiencies, selenium deficiencies are frequently seen due to poor nutrient status in modern-day soil.
Selenium is a wonderful treatment for autoimmune thyroiditis, assisting in lowering antibody levels. In addition, it also is used to convert T4 to T3, helps regulate reactive oxygen species to prevent damage to the thyroid gland, and can improve thyroid structure seen on ultrasound imaging.
Standard doses of selenium range between 200-400mcg per day. This should not be exceeded due to risk of toxicity. Selenium toxicity may occur if supplementation exceeds these levels and lead to vomiting, diarrhea, tremors, and other unwanted symptoms.
Naturally, selenium may be increased through the consumption of 4-6 Brazil nuts per day. That said, concentrations of selenium may vary!
Now that hypothyroidism treatments have been established, we can dive into the conventional and natural solutions to hyperthyroidism as well!
While there are multiple treatments for hyperthyroidism, there is one main one to discuss. This is methimazole, a first-line hyperthyroidism treatment commonly used prior to radioactive iodine therapy or thyroid surgery.
Methimazole inhibits the production of thyroid hormones by blocking iodine from binding thyroglobulin to form thyroid hormones. Common side effects are nausea, vomiting, headaches, drowsiness, dizziness, rashes, and hair loss. Rarely, adverse side effects such as agranulocytosis and hepatotoxicity may occur.
Iycopus virginicus (Bugleweed)
This is an herb frequently used for its thyrosuppressive effects. Lycopus not only acts as a TSH receptor antagonist but also inhibits the production of T4 (therefore lowering T3 levels). In addition, it decreases Grave’s Disease activity by blocking antibodies from binding. This herb should not be taken during pregnancy, lactation, or hypothyroidism.
Lithospermum ruderale (Stoneseed)
This is another thyrosuppresive herb that is frequently used in medicine to treat hyperthyroidism and Grave’s Disease. Lithospermum inhibits TSH production, TSH binding, and the secretion of thyroid hormones. It is contraindicated in pregnancy, lactation, hypothyroidism, and liver disease.
Melissa officinalis (Lemon Balm)
This is yet another popular thyrosuppressive herb that is used in natural management of hyperthyroidism. Melissa officinalis has a similar mechanism of action as Lycopus virginicus. It inhibits the production of T4 and slows TSH-driven stimulation of the thyroid.
I often use all three of these herbs simultaneously for their synergistic properties!
Eating a clean diet free of inflammation-causing foods is important for management of all autoimmune conditions. A clean diet helps to lower antibodies and therefore resolve symptoms and decrease disease process.
Elimination diets are the gold standard for determining which foods should be eliminated based on your individual needs. Gluten is known to aggravate autoimmune thyroiditis, so a gluten-free diet is therefore regularly recommended for optimal management of these conditions.
Finally, I wanted to share with you my favorite supplements for thyroid health. To make it easy for you, I’ve also supplied the links to purchase them directly from my store.
To order supplements from my store, you have to create a patient login. You can follow the ‘Welcome Link’ I’ve supplied below to do this! Current patients already have an account and will not need to go through this process.
Once you set this up, you will be able to follow the links to the supplements listed and purchase them. Once you set up your account, you will be able to easily order products recommended in future articles as well. Plus, you won’t miss out on Natural Med Doc supplement discounts and promotions!
The Welcome Link: https://us.fullscript.com/welcome/sbennett1527799795
Without further ado, here are my favorite supplements to support thyroid health:
Priority One Thyroid Support is a complete vegetarian supplement supplying all the essential nutrients to promote healthy thyroid function. The standard dose is two capsules a day or as directed by a naturopathic physician.

Vital Nutrients Selenium is a potent antioxidant that supports normal cell function. Selenium is a trace element that is essential in the body in small amounts. It helps cells function normally by supporting the actions of several enzymes, particularly antioxidant enzymes and those involved in thyroid hormone metabolism. Selenium also supports the body’s immune system! You will need to take 1-2 capsules daily or as directed by a practitioner.

RTL Labs i-Throid is a superior iodine formulation created to enhance thyroid treatment and offer long-term, consistent results. i-Throid contains the ideal balance of iodine and free elemental iodine which is highly absorbable and binds with tyrosine to produce thyroid hormones.
i-Throid works synergistically with Nature-Throid and a-Drenal to offer a well-rounded, highly effective thyroid treatment protocol. Serving size is one capsule or as directed by your doctor.
Phew! That’s a wrap for everything you need to know about thyroids, including hyper and hypothyroidism treatments and diagnosis.
To recap, we covered:
I sincerely hope that this article has given you a better understanding not only of the thyroid and thyroid dysfunctions in concept, but also pertaining to your personal life! Of course, I always hope you will reach out and book a free consultation if you have any additional and specific questions about your thyroid concerns!
What did you learn about your thyroid today? Did anything surprise you? Did you still have any burning questions? Talk to us and we can start a conversation!
Hello, my name is Dr. Sarah Bennett, NMD!
I am a naturopathic physician licensed in the state of Arizona currently practicing at my office in Scottsdale, AZ. I received my degree from Southwest College of Naturopathic Medicine, did a year residency at Keystone Natural Family medicine, and received additional training for aesthetics & anti-aging at National Laser Institute.
My passion and fascination for natural medicine began during my undergraduate studies at Indiana University where I got a dual degree in neuroscience & psychology.
I saw how a preventative approach could help you live a long and youthful life. Since then I have dedicated my life to serving others to understand the latest medical trends.
I spend my spare time running, hiking, rock climbing, camping, testing out new diets, and reading books on latest medical trends / listening to podcasts to find the latest nuggets of knowledge to improve the quality of life for my patients. I look forward to serving you!