By Dr. Sarah Bennett, NMD / March 23, 2020
Hormonal concerns effect millions of men and women world wide. This is one of the reasons that hormone replacement therapy is so widely practiced.
PCOS, or polycystic ovarian syndrome, is the most common hormonal disorder in young women. In fact, it affects at least 116 million women worldwide!
PCOS is an incredibly emotional diagnosis for many women… feeling as though you have been sentenced to a life long battle with weight gain, insulin resistance, acne, hair loss, and infertility.
Chances are, if you’ve stumbled upon this article, you or someone you know has this diagnosis. There are likely many unanswered questions and confusion about how this complicated condition actually effects the body.
This is exactly why I wrote this article! To shed light on exactly how this condition effects the body and discuss conventional and natural treatment options. The purpose of this article is to help women reverse their PCOS, making what seems impossible, possible!
So let’s get straight to it! How does PCOS effect the body and how do you REVERSE it?
PCOS is often characterized as a hyperandrogenic condition causing women to gain weight, have acne, experience hair loss on the scalp and thick hair growth on the face. Women often times have significant mood swings, suffer from irregular or absent menstrual cycles, and frequently struggle with infertiliy
This diagnosis may mean you have to be more careful with things like the food you eat, amount of exercise you get, and medical check-ins… but it doesn’t have to be a life sentence. Yes, you can reverse your PCOS! And we will discuss how in this article.
More recently, the definition and criteria defining PCOS have continued to broaden as we gain knowledge on the disease process and recognize different phenotypes – or presentations – of the condition. In other words, not all women will have the symptoms listed above!
To help you better understand what all this means, I will soon discuss the different phenotypes. This should help you better determine which type you likely have. I will also outline the key contributing factors to PCOS, risk factors of developing PCOS, comorbid conditions, and the conventional and natural treatment options available.
As a bonus resource, much of the information in the article comes straight from the book 8 Steps to Reverse Your PCOS by Dr. Fiona McCulloch N.D., an expert in reversing PCOS. (1) if you have been diagnosed, I highly recommend reading it!
PCOS is a hyperandrogenic condition that affects fertility, metabolism, cardiovascular health, skin, and mood. Recently, it has been more clearly defined as the following criteria:
PCOS has 2 of the 3 signs and symptoms listed below:
This criteria is broad and leaves room for overdiagnosis of the condition, categorizing PCOS as a diagnosis of exclusion. This means that all other conditions that could cause the same symptoms must first be ruled out.
Based on this criteria, there are 4 phenotypes of PCOS, listed in the diagram below.
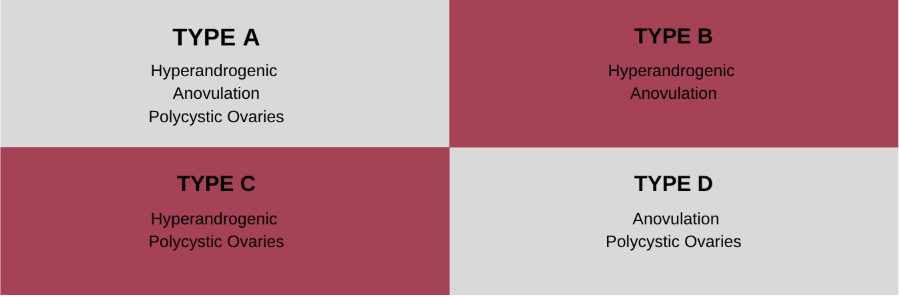
For optimal treatment, it is important to determine which type of PCOS you have. Don’t worry if it seems overwhelming… I’ll help you figure it out!
Each type is positive for 2 of the 3 criteria, therefore to begin this process, just determine which of the criteria fit you. Each type has a different myriad of symptoms, so next you will compare yours to the lists below.
60% of all PCOS patients
Type A is the classic form of PCOS… and also the most common and severe. Women in this category often have the strongest genetic predisposition for PCOS.
As women age and begin to reverse their PCOS using these methods, they are able to move to less severe types of the disorder and – eventually – reversal.
The common symptoms that are experienced by women with this type of PCOS include:
8.4% of all PCOS patients
Type B is another classic form of PCOS. It also presents very similarly to Type A. The main difference is that polycystic ovaries are not present in Type B. This type consists primarily of older women who may have outgrown Type A.
The common symptoms that are experienced by women with this type of PCOS include:
Type C, also known as Ovulatory PCOS, is a milder non-classic type of PCOS. Women who successfully manage weight, insulin resistance, and inflammation may move from Type A to Type C.
The most characteristic traits of this type of PCOS include:
Type D is a non-classic form of PCOS as well as the mildest in presentation. This type is controversial in nature as some may disagree that this qualifies as PCOS. I agree with Dr. Fiona McCulloch N.D. and include this in the types of PCOS to be diagnosed. These women do not have overtly elevated androgens and often do not present with hyperandrogenic symptoms.
The most characteristic traits of this type of PCOS include:
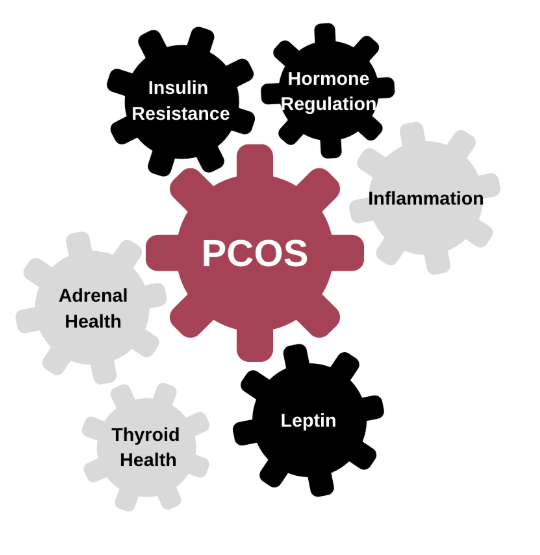
To thoroughly understand PCOS at its core, we have to look at the physiological process that is associated with the disorder.
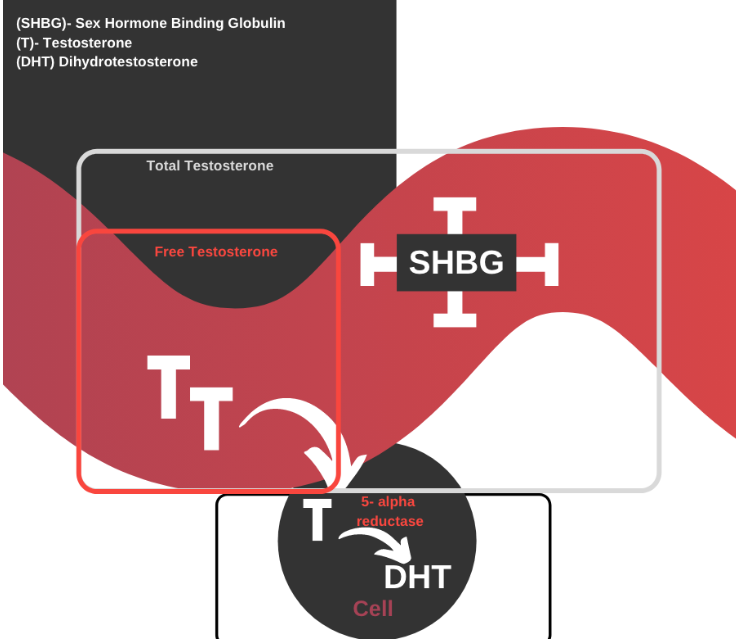
Even though excess androgen production is a hallmark characteristic of PCOS, the majority of women with PCOS have total testosterone levels within normal limits. This is why it is important to test more than just total testosterone, as there are many different androgens and levels that should be checked.
Androgen production in PCOS may be adrenal dominant or ovary dominant, both producing hyperandrogenic symptoms (also known as hirsutism) and possibly virilism.
The androgens to become familiar with are listed below:
Theca cells produce testosterone in the ovaries. These cells make up the outer layer of the ovaries, become thick, and begin to produce increased amounts of testosterone in PCOS. This production of testosterone is stimulated by elevated insulin and inflammation levels.
The adrenal glands are a triangular shaped gland that sits on top of our kidneys. The outer layer cortex of the adrenal gland produces our primary stress hormone cortisol and androgens in the form of DHEA and testosterone.
The production of androgens from the adrenal glands is primarily stimulated by stress, which is problematic since many women with PCOS have a heightened stress response.
To determine this, have your provider run your testosterone levels and DHEA-S levels. If the ratio of testosterone to DHEA-S is greater than 4.4, it is likely you produce the majority of androgens from your adrenal glands.
It has been found that women with PCOS who have adrenal dominant androgen production have lower metabolic and cardiovascular risk potential due to the anti-aging and anti-inflammatory effects of DHEA. (2)
Androgens at healthy levels are important for maintaining libido, muscle mass, energy, cognitive sharpness, and more… But in excess, androgens cause hirsutism (acne, male pattern hair growth, male pattern baldness) and viralism (elevated sex drive, enlarged clitoris, deepening voice, amenorhea, increase muscle mass).
Women with PCOS have a heightened stress response (enzymatic pathway that is upregulated), often having increased levels of anxiety that result from increased production of our primary stress hormone cortisol. (3)
Symptoms associated with elevated cortisol:
Over time, chronic stress and hyperactive cortisol production may lead to HPA axis dysfunction.
Symptoms associated with low cortisol and HPA axis dysfunction:
Studies have shown risk factors for having increased cortisol production include things like PCOS, increased BMI, nodules in the pituitary gland, and drug use. (5,6)
Elevated cortisol production disrupts hormone production and efficacy, weight gain, mental emotional stability, and thyroid hormone production.
If you are interested in learning more about cortisol regulation and dysfunction, I’ve written an entire article on cortisol here!
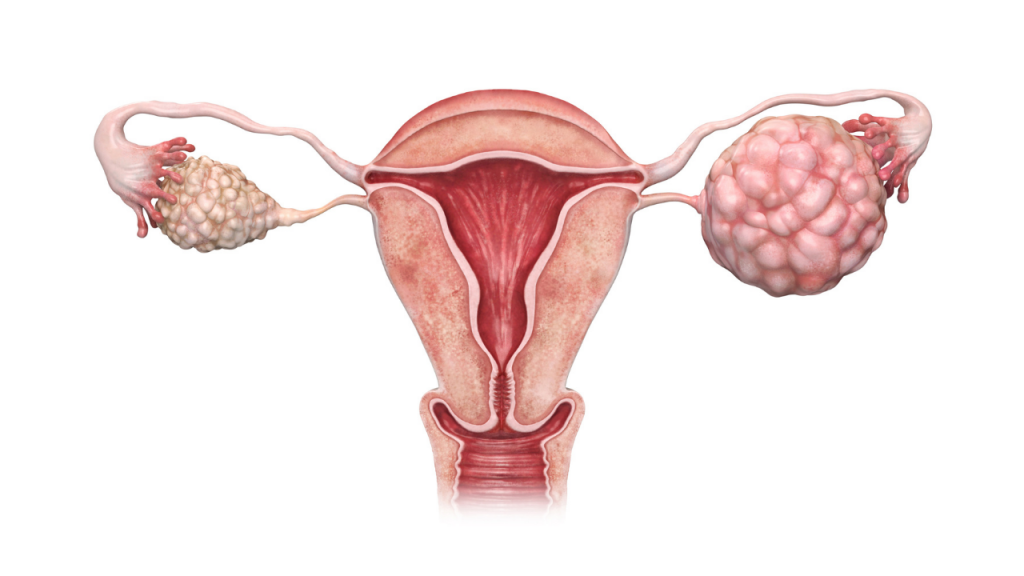
Polycystic ovaries do not actually contain true cysts, or fluid-filled sacs that often burst and cause immense pain. Polycystic ovaries just look like they contain many cysts, often described as looking like a bunch of grapes or a string of pearls.
This appearance is caused by partially developed follicles or eggs residing in the ovaries and building up over an extended period of time. This accumulation of effects is a vicious cycle. The outer layer of the ovary, known as the theca produces testosterone.
In PCOS this layer thickens, increasing production of testosterone and stalling the folliculogenesis. (7) This causes the follicles to accumulate. Elevated levels of insulin will also contribute to this effect, which is another feature commonly seen in PCOS.
As you can imagine, this finding is more common in younger women, often aged 15 to 35, due to abundant follicle counts. As women age, follicle counts naturally begin to decline, decreasing the likelihood of finding polycystic ovaries on ultrasound results.
That being said, it is more common to find polycystic ovaries on ultrasound results of younger women.
There are 3 phases of the female menstrual cycle: follicular, ovulation, and luteal. The first full day of menstrual flow is considered day 1 of the menstrual cycle.
Day 1 until ovulation is considered the follicular phase. During this time, follicular stimulating hormone (FSH) is elevated, developing 3- 30 follicles which each house eggs. Additionally, estrogen begins to rise, building the lining of the uterus.
Ovulation is 1 single day, usually around day 14. Ovulation phase begins when both estrogen and luteinizing hormone (LH) surge, causing the follicle to rupture and release the egg for fertilization.
The luteal phase begins after ovulation, lasting through day 28 of the cycle or until the start of the next menstrual cycle. During the Luteal phase, the ruptured follicle forms the corpus luteum which begins to produce higher quantities of progesterone.
Elevation in progesterone and estrogen during this time increases thickening of the endometrium to prepare for implantation of a fertilized egg. If there is no implantation, the corpus luteum degenerates, resulting in a drop in hormone levels stimulating the shedding of the lining of the uterus (the next menstrual cycle).
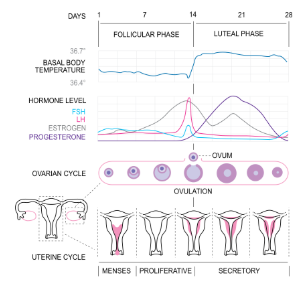
Oftentimes this cycle is disrupted in women with PCOS, causing delayed or anovulation and irregular or absent menstrual cycles. Signals for proper hormone production are disrupted, inhibiting not only ovulation but also overall hormone production.
Gonadotropin releasing hormone (GnRH) is produced from the hypothalamus to signal the production of FSH and/or luteinizing hormone (LH) from the pituitary gland. This then stimulates the matureation of the follicle and sex hormone production respectively.
GnRH pulses slowly in the follicular phase, stimulating the release of FSH for maturation of the follicle, and more quickly to stimulate the release of LH to signal the production of sex hormones. In women with PCOS, GnRH is improperly regulated, pulsing more quickly and stimulating the release of androgens.
The follicle contains 2 types of hormone producing cells: theca and granulosa cells. As seen below, theca cells produce androgens and granulosa cells produce estrogens. In PCOS, the follicle contains a thickened theca layer which responds to elevated LH and insulin by producing excess androgens.
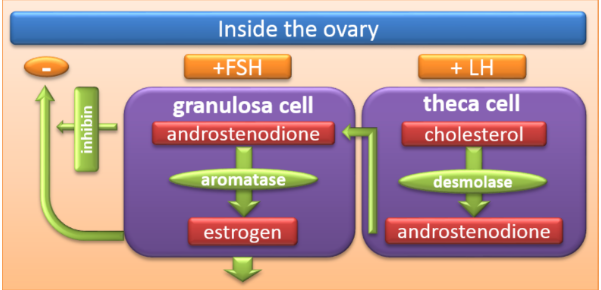
Due to the fast pulsing GnRH, elevated LH, and thickened theca layer, there is slow maturation of follicles, not enough estrogen surge to stimulate ovulation, and small or no corpus luteum for proper production of progesterone.
This results in not only infrequent or absent ovulation but also improper estrogen and low progesterone production. Without a late cycle drop in progesterone and estrogen levels, menstrual shedding will fail to occur, causing infrequent or absent menstrual cycles.
Inflammation is a key factor for disease progression in PCOS, and is imperative to address in order to reverse PCOS symptoms. Inflammation is a term frequently referenced, yet rarely explained. What is inflammation and what causes it?
In a healthy body, inflammation is a natural response to injury or illness. Inflammation is a response stimulated by signaling chemicals such as cytokines and prostaglandins. These chemical signals induce the production of white blood cells to repair injury and fight off injury.
In PCOS, this system does not function properly. Cytokines are secreted at a low level consistently causing a constant low-grade inflammation.
To make things worse, this dysfunction is exacerbated by the often increasing accumulation of adipose tissue, or fat cells. Fat cells store excess calories, or energy intake. At a certain point these fat cells fill, and begin spilling the excess free fatty acids into the bloodstream. (8)
Unable to be used by other cells, these free fatty acids begin to cause tissue and organ damage. (9) This damage stimulates the release of immune cells to begin the healing process which further increases inflammation levels.
And that’s not all… Adipose tissue has poor blood flow, and therefore when adipose tissue has accumulated in large amounts, the central cells do not receive proper nutrients and begin to die.
This cell death is referred to as fat necrosis, and further stimulates the inflammatory immune response to begin cleaning the necrotic cells. (10)
This chronic inflammation impairs insulin sensitivity, increasing weight gain and creating a vicious cycle. (11) It also disrupts hormonal production, quality of eggs, and will stimulate premature aging.
Insulin resistance is strongly associated with not only PCOS but also obesity. Insulin is a signaling hormone released from the pancreas that stimulates the cells to take up glucose from the blood for storage or immediate use.
Simple carbohydrates and sweets are easily and directly converted to glucose in the blood. In response to frequent intake of these foods, blood glucose levels are regularly elevated, stimulating the pancreas to secrete high levels of insulin.
Chronically elevated insulin over time causes cells to stop responding. This begins the cycle. This creates a rising blood glucose level, which stimulates the pancreas to then begin producing more and more insulin, which further desensitises cells.
Research has linked elevated insulin levels and insulin resistance to the development of obesity, which is also characteristically seen in PCOS, and also a key factor that aggravates symptoms. (12)
Generally, insulin resistance is a product of first eating high quantities of simple carbohydrates and sweets, but this is not necessarily the case for PCOS. The development of insulin resistance in PCOS is the result of the combination of genetics, intake of simple carbohydrates, lipotoxicity, and chronic inflammation.
Insulin resistance in turn increases obesity, inflammation, lipotoxicity, and increases production of testosterone from the ovaries, just further contributing to this cycle.
This brings me to leptin, a signaling hormone produced by fat cells. When insulin levels are high, glucose is stored in fat cells, which in turn secrete leptin. Leptin signals to the brain that energy levels are high and storage is full, thus inhibiting appetite.
The higher the body fat percentage, the higher the leptin production. Similar to insulin, leptin resistance begins to develop over time. The brain stops responding, and therefore appetite is uncontrolled, leading to excess hunger, overeating, increased insulin production, lowering metabolism, and elevation in body fat percentage.
In addition, research has found that leptin resistance interferes with proper hormone production by inhibiting the production of FSH. (13) Therefore, leptin is another vital piece of the puzzle that must be addressed to reverse your PCOS.
Finally, we arrive at thyroid health. Optimal thyroid hormone production is essential for maintaining a healthy metabolism, energy, mood, cognitive ability, bowel movements, etc. Yet around 10 million Americans are estimated to suffer from hypothyroidism, and a diagnosis of PCOS significantly increases risk of thyroid dysfunction.
Women with PCOS are 2.87 times as likely to develop subclinical hypothyroidism, 65% more likely to develop Hashimoto’s Thyroiditis, 26.6% more likely to have a goiter… So how does PCOS increase your risk of thyroid dysfunction?
Studies have shown that elevated insulin, inflammation, and leptin levels inhibit thyroid production and healthy conversion of T4 to T3. As explained above, these levels are characteristically elevated in women with PCOS.
In times of physiological stress, such as injury, illness, metabolic dysfunction, and mental emotional stress, conversion of T4 to T3 is decreased while conversion of T4 to reverse T3 (RT3) is increased, causing what is known as Low T3 syndrome, or euthyroid sick syndrome.
RT3 is the third most abundant thyroid hormone in the body, created primarily in the peripheral tissues. RT3 is metabolically inactive and will compete for the same receptors as metabolically active T3.
Elevating T4 conversion to RT3 is your body’s way of lowering your metabolism and putting your body into a state of hibernation. While this is the body’s defense mechanism to protect tissues from excess metabolic stimulation in times of disease or low caloric availability, it also contributes to an increase in hypothyroid symptoms.
But that’s not all… This is also a vicious cycle. Thyroid hormones regulate lipid and glucose metabolism. Subclinical and overt hypothyroidism and hyperthyroidism impair lipid and glucose metabolism, increase insulin resistance, contribute to worsening symptoms of PCOS, and ultimately increasing risk of cardiovascular disease. (14)
This is why it is essential for providers to do a thorough thyroid panel for all PCOS patients.
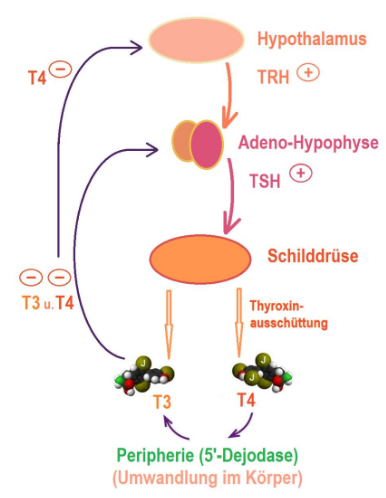
TSH- Thyroid stimulating hormone is a signalling peptide produced by the pituitary gland to sygnal the thyroid gland to produce more thyroid hormones when systemic levels begin to drop.
FT4- Thyroxine or T4 is the most abundant thyroid hormone in the body. The majority of T4 is bound to proteins in the bloodstream, and therefore is unable to be used by cells. Free T4 (FT4) is what is metabolically available to be used by your cells at any given time, and therefore is the most accurate value to assess T4 status.
FT3- Triiodothyronine or T3 is the most metabolically active thyroid hormone and is primarily produced in the peripheral tissues through conversion of T4. Free T3 (FT3) measures what is metabolically available for cells to use and therefore is a more accurate value for thyroid hormone status.
RT3- Reverse T3 (RT3) is an isomer of T3 produced in abundance in time of high physiological stress. RT3 is much less metabolically active than T3 and therefore puts the body into a hibernation state when elevated, creating increased presentation of symptoms associated with hypothyroidism. For disease management, prevention, and treatment of unwanted symptoms, this value is essential to assess!
Antibodies- PCOS has a strong comorbidity with development of other autoimmune conditions, and 90% of adult hypothyroidism is associated with an autoimmune cause… This makes it very important to test thyroid antibodies for optimal management. Studies have shown an increased prevalence of elevated thyroid peroxidase (TPO) antibodies and thyroglobulin (TG) in women diagnosed with PCOS.
Now that we’ve established all that you need to know about what PCOS is and how it works and impacts your body, we can start diving into the treatment options!
I always feel like the best place to start is with conventional treatment methods since this is likely what people are most familiar with and used to. That said, I will soon also go into natural remedies for PCOS so that you know you have options and can see how you can go about reversing your PCOS naturally!
The first area we will look at reversing conventionally will be the inflammation and autoimmunity. The standard treatment for this is Prednisone.
Prednisone is a corticosteroid medication frequently used to suppress inflammation and immune function. It is frequently prescribed for management of autoimmune conditions and inflammatory conditions such as rheumatoid arthritis, lupus, bronchitis, asthma, etc.
Be cautious before starting this medication as it has many harmful side effects including weight gain, increased blood sugar, thinning skin, insomnia, and (if used long term or in high doses) dependency.
The next area that is addressed in cases of PCOS is concerns regarding insulin levels and lipids. Metformin and Statins the conventional medications for this area.
Metformin is an antihyperglycemic agent frequently used in diabetes mellitus type 2 to control blood glucose levels. It effectively decreases glucose absorption from the intestines, gluconeogenesis from the liver, and improves insulin sensitivity.
Metformin’s active constituents buformin and phenformin are isolated from french lilac. More recently Metformin has been classified as a safe anti-aging medication with many health benefits, such as increasing longevity, decreasing cancer risk, improved cardiovascular health, and more.
Statins such as lipitor are classified as HMG-CoA reductase inhibitors, which are prescribed to lower cholesterol levels and improve cardiovascular health. The benefit of statins is controversial as statins have been shown to increase risk of diabetes, muscle pain and degeneration, and increase liver function tests.
In addition, Statins inhibit the production of cholesterol, but also CoQ10 which is essential for muscle health and glucose metabolism.
Hormonal contraceptives are the most frequently prescribed medication to women of ovulating age for everything from contraceptive purposes, to acne, or menstrual cycle irregularities.
Hormonal contraceptives contain synthetic progestins and estrogens that override natural hormone production, balanced or dysfunctional. When taken exogenously, these synthetic hormones decrease the body’s natural production of progesterone and estradiol, often but not always leading to negative side effects. (15)
Research has linked oral contraceptives to increased panic disorder and depression in susceptible individuals.(16, 17)
On a more serious note, oral contraceptives have been linked to an increased risk of cardiovascular disease, thrombosis, and breast and cervical cancer. (18, 19, 20) This being said, studies have shown that oral contraceptives can also protect against endometrial cancer which is important for women with PCOS.
PCOS accounts for 80% of anovulatory infertility cases. (21)
Clomiphene is a fertility medication categorized as a selective estrogen receptor modulator (SERM) used to induce ovulation. Side effects include pelvic pain, hot flashes, nausea, vomiting, trouble sleeping, ovarian cancer, and seizures. It has been found that 15% of women with PCOS will not respond to the max dose of clomiphene.
Letrozole is an aromatase inhibitor, inhibiting the conversion of testosterone to estrogen. It is often used in place of clomiphene due to a lower side effect profile.
Finally, there are two main treatment options for the androgen concerns related to PCOS. These are Spironolactone and Finasteride.
Spironolactone is a potassium-sparing diuretic often prescribed for blood pressure control, but in the case of PCOS it is prescribed for its anti-androgen effects.
Spironolactone effectively reduces the androgen count as it is the antagonist of the androgen receptor, blocking it and thereby inhibiting the effects of androgen on the body.
Finasteride is a 5-alpha reductase inhibitor prescribed for its anti-androgen effects. It is generally prescribed for androgenic hair loss and enlargement of the prostate, but may be used to decrease androgens in PCOS.
Finally, I know many of you are concerned about a lot of synthetic or conventional treatment options available and are seeking advice in terms of natural remedies for PCOS.
This is where I come in to help! I’ve compiled a comprehensive list of important natural remedies for PCOS management so that you have an excellent place to start. Of course, it is also always important to make sure you talk through these decisions with your naturopathic doctor.
If you don’t have a regular go-to resource already, you can also always reach out to me and schedule a free consultation! I’d more than willing to help guide you to your next steps in natural PCOS management.
To make it especially easy for you, I’ve also supplied the links to purchase them directly from my store whenever available so you know you’re getting the exact recommendation I provide. Plus, you won’t miss out on Natural Med Doc supplement discounts and promotions! To order supplements from my store, you simply have to create a patient login and click through the site!
To do this, you will need to follow the ‘Welcome Link’ I’ve supplied below. Current patients already have an account and will not need to go through this process, so you only need to set everything up once and you’re set!
Welcome Link: https://us.fullscript.com/welcome/sbennett1527799795
My favorite Supplements and prescriptions for managing PCOS:
Low Dose Naltrexone
Naltrexone is a prescription commonly used in standard doses ( 50 mg or more ) to bind the endogenous opioid receptors in treatment of addiction. More recently, low doses of naltrexone are being used for its gentle effect on inflammation and immune function.
Low dose naltrexone (LDN) has been found to act as a glial cell modulator, decreasing microglial production of inflammatory factors such as cytokines, substance P, nitric oxide, etc. (22) Many inflammatory and pain conditions involve chronic activation of these immune cells.

Vitamin D
As you may have heard, Vitamin D is an excellent way to boost your immunities and help with a variety of different concerns.
Hi-Po Emulsi-D3™ is a concentrated, highly bioavailable liquid vitamin D formulation offering a broad range of dosages and titration possibilities. Unlike most other liquid vitamin D products available, Hi-Po Emulsi-D3™ is a convenient, pleasant-tasting and easily-mixed formula.
A natural emulsion technology allows for the production of a 2000 IU per drop formula that quickly and completely disperses in liquid. This cutting edge technology provides enhanced bioavailability utilizing only naturally derived ingredients that are free of preservatives and synthetic surfactants.
Presented in a 1oz glass bottle, Hi-Po Emulsi-D3™ makes dosing vitamin D convenient. It can be dropped into any beverage or simply put on the tongue, providing accurate dosing 1 drop at a time.
As a dietary supplement, take one drop per day, or as directed by your health care practitioner.

Berberine
Berberine belongs to a class of naturally occurring alkaloids found in the roots, rhizomes, and stem bark of a number of plant species.
Studies with berberine in people with diabetes show that it exerts multiple beneficial effects on glucose and lipid metabolism. Naturally derived berberine is provided as berberine hydrochloride, the best-studied form.

Myo-Inositol
Myo-inositol is a naturally-occurring inositol isomer. (23) It helps promote the activities of the ovaries through its role as a precursor to inositol 1, 4, 5-triphosphate (InsP3), which regulates menstrual cycle hormones and oocyte maturation. (24, 25, 26) This means that it can also be used along with the supplements in the ovulation and menstrual regularity section below!
Myo-inositol also promotes healthy glucose metabolism through the production of inositolphosphoglycans (IPG), signaling molecules involved in insulin-dependent glucose uptake. (25, 26)
In a clinical trial involving 42 women, participants were randomized to consume 400 mcg of folic acid alone or in combination with 4 g of myo-inositol daily for six to eight weeks. When compared to the placebo folic acid treatment, myo-inositol supplementation better promoted hormonal balance, menstrual regularity, and insulin sensitivity. (24)

L-Theanine
L-Theanine is a unique amino acid blend that helps promote relaxation without causing drowsiness. I-Theanine may also ease occasional nervous tension and irritability.
Green tea has been recognized for centuries as having relaxant properties. L-Theanine, a unique amino acid derived from tea, provides the characteristic taste of green tea. L-Theanine has also been discovered as the biologically active constituent of green tea responsible for promoting relaxation.
In a preliminary non-clinical study, an L-theanine solution enhanced alpha wave production in the occipital and parietal regions of the brains of volunteers. These observed patterns are considered to be an index of relaxation.
Furthermore, it did so rapidly and without causing drowsiness. In two additional studies, alpha waves were also shown to be detectable soon after l-theanine administration.
Theanine is also useful for supporting healthy cellular function. Preliminary research suggests that l-theanine may be helpful for premenstrual support including healthy mood. Furthermore, theanine has been reported to moderate the effects of caffeine on the central nervous system.
L-Theanine’s safety is supported in studies and by its long history of safe consumption in tea. Pure Encapsulations L-Theanine is Suntheanine®, the brand which has been used in scientific studies.

Phosphatidylserine
Phosphatidylserine supplies a supplemental source of this important phospholipid, which is a structural part of biological membranes. Phosphatidylserine is involved in signal transduction activity, and may positively impact cognition.

St. Johns Wort
St. Johns Wort (Hypericum perforatum) and its active constituent, hypericin, help to increase one of the brains neurotransmitters, serotonin, by blocking the action of mono-amine oxidase (MAO), the enzyme responsible for breaking down serotonin, and by impairing the uptake of serotonin into nerve cells.
Clinical studies with St. Johns Wort extract have demonstrated that this herb helps support normal psychological mood.

Rhodiola
Herb Pharm prepares their Rhodiola Extract from the dried root of Rhodiola rosea plants which are Certified Organically Grown and/or Sustainably Wildcrafted in their natural habitat.
To assure optimal extraction of Rhodiolas bioactive flavonoids and delicate rose flavor, the root is hand-harvested at its optimal potency and carefully shade-dried.

Bio-Identical Progesterone
Progesterone, a hormone derived primarily from the corpus luteum and secondarily from the adrenal gland and the male testes, is a precursor hormone which can be converted, as required, into other steroid hormones such as DHEA, estrogen, androstenedione, testosterone, and cortisol.
Using a bio-identical hormone remedy is an excellent way to help treat hormonal concerns within your body!
Karunas Progesterone Pure is specifically designed for two populations: (1) male patients who may benefit from the supportive actions of progesterone and (2) all people suffering with skin sensitivities or allergies.
Progesterone, being a small, fat-soluble molecule, is easily absorbed through the skin. For general application, skin sites recommended include the inner areas of the thighs and arms, neck, upper chest and abdomen. The site should be rotated daily for maximum absorption. Allow 2-3 months for maximum effect.

Vitex
Vitex 750 contains high dose Vitex Extract that is fortified with Vitex Essential Oil making it a powerful clinical tool to support women during times of hormonal change.
Vitex is excellent in supporting normal ovarian function, helping to maintain healthy hormone levels, and helping to promote healthy moods during the menstrual cycle.
Dioscorea Villosa
Traditionally used in Herbal Medicine, Dioscorea villosa can help relieve typical menstrual symptoms and to promote digestive comfort. It is also commonly prescribed to help with areas like ovulation and menstrual regularity.

Herb Pharms Saw Palmetto assayed extract is prepared from the ripe berries of Serenoa repens palms that have been Sustainably Wildcrafted in their native habitat.
This is an excellent supplement in terms of controlling androgen excess. Plus, it’s gluten-free and completely compatible with a gluten-free diet!

Paeonia lactiflora is a herbaceous perennial flowering plant that is native to central and eastern Asia. It can be found from eastern Tibet across northern China to eastern Siberia.
In terms of health, it can be used for everything from androgen excess to gout, cough, osteoarthritis, and more.

Glycerrhiza glabra aids the treatment of arthritis, asthma, gastrointestinal ulcers, stress, irritable bowel syndrome, gout, eczema, and bronchitis.
You may be more familiar with it as licorice! The sweet flavor is extracted from the same plant to make the candy everyone knows and loves.
I know that was a lot to take in, but it is my hopes that this will serve as your one-stop guide to understanding everything you need to know about PCOS, including PCOS treatment, diagnosis, and medication.
To re-cap, the areas that we covered today include:
Whether you are diagnosed with PCOS or you are simply suspicious that you are exhibiting symptoms, I hope that this guide makes the journey easier for you. It can be incredibly emotional and confusing, especially with all of the stigma and stereotypes you may find on the internet.
Do you have tricks you use to manage your PCOS symptoms? How will you employ the advice in this guide so that you can turn your life around?