By Dr. Sarah Bennett, NMD / March 12, 2020

Diets are hard. Diets when you have medical concerns, disorders, or dysfunctions like hypothryoidism can feel impossible.
Fortunately, we have some advice tailored specifically to people like you. The diet for optimal thyroid health involves increasing nutrients that act as co-factors for proper production of thyroid hormones and eliminating foods that cause inflammation and aggravation of potential autoimmunity.
And on that note… did you know that 90% of adult hypothyroidism is associated with an autoimmune cause? And just like with other autoimmune conditions, diet and lifestyle are an essential part of disease management.
But before we dive into what foods to eat or avoid, make sure you are open about your choices with your doctor if you are currently taking thyroid medication. For proper absorption of thyroid medications, it is vital to take them on an empty stomach in the morning upon waking up and to wait one hour before eating or taking medications/supplements. This is because thyroid medications are easily bound by minerals and medications in the stomach like iron, calcium, chromium, and bile-salts.
All that out of the way, let’s dive into the best diet for hypothyroidism by highlighting which foods you should eat and avoid (as well as some bonus personal recommendations by yours truly).

To kick things off, I always think it’s best to get the less fun part out of the way: the foods that you should be avoiding and aiming to cut out of your diet.
No matter what diet you are on, this part is never easy. Especially if you have to give up foods that you are used to enjoying regularly. But soon, we can dive into the foods that you should make a point to add to your diet, and a lot of them can make for fantastic replacement meals once you adjust to the changes!
Gluten-free products are everywhere! If they can slap a gluten-free sticker on it, they will…
Trendiness aside, there is a reason it is such a popular concept. There are many health benefits to eating a gluten-free diet, and thyroid health is among them.
Gluten is a protein naturally found in wheat, barley, rye, and oats. That said, beware… modern foods are now using gluten as an additive for flavor or thickening purposes, so it can be found in some unexpected places as well!
This modern increase in gluten consumption is associated with the development and aggravation of many diseases. Most notably, it will cause an autoimmune condition called celiac disease in genetically pre-dispositioned people!
Celiac disease is an autoimmune condition resulting in damage to the lining of the small intestine caused by the ingestion of gluten. Research has shown that having celiac disease increases the risk of developing autoimmune thyroiditis by a shocking three times (and vice versa)!
In addition, the prevalence of both thyroid conditions and celiac disease is rising. What is the connection? Could the increased consumption of gluten be a contribution…?
Research has shown that in many cases, a strict gluten-free diet over the course of a year can singlehandedly reverse subclinical hypothyroidism. This suggests that gluten actually has a huge impact on the disease process in hypothyroidism.
So… how does gluten actually affect thyroid function?
In celiac and non-celiac gluten-sensitive individuals, gluten consumption leads to increased intestinal permeability. Increased gut permeability is often associated with autoimmunity. Due to this increased gut permeability, gliadin, a component of gluten, is now able to seep through the tight junctions in the intestinal lining, stimulating an immune response that creates antibodies against the foreign material.
The gliadin molecule is similar to that of transglutaminase, causing the production of gliadin and transglutaminase (tTg) antibodies. Both of these antibodies have been found to attack the thyroid follicles and extracellular matrix due to its high concentrations of transglutaminase.
Although gliadin and tTg antibodies are traditionally a marker for Celiac’s Disease, a high percentage of patients with autoimmune thyroiditis display elevated titers of tTg antibodies. This has been shown to positively correlate to the level in thyroid peroxidase (TPO) antibody titers. These findings suggest that celiac antibodies contribute to the development of autoimmune thyroiditis and therefore should be tested in all autoimmune thyroid dysfunction patients.
Ultimately, gluten is associated with the aggravation and development of autoimmune thyroiditis. Since 90% of hypothyroid cases are associated with an autoimmune cause, it is imperative to remove gluten from the diet.
I know this one will hurt some of you… sugar substitutes seem like such an easy way to enjoy the same sweetness of sugar with magically no calories… often, if things seem too good to be true, they are.
Artificial sweeteners, specifically sucralose, have been shown to decrease thyroid function. Sucralose disrupts the pituitary thyroid access, decreasing TPO, TSH, and thyroid hormone production.
What does that mean? These include things like cabbage, cauliflower, broccoli, turnips, spinach, brussels sprouts, mustard greens, and kale. These are well-known goitrogens that contain thioglucosides.
That’s a lot of big words. Goitrogens are chemicals, nutrients, and dietary supplements that contribute to enlargement and dysfunction of the thyroid through decreasing thyroidal iodine uptake.
Once the cruciferous vegetables are metabolized to thiocyanates, these compounds inhibit iodine transports and incorporation of iodine on the thyroglobulin molecule. In turn, thyroid hormone production is diminished and TSH increases.
Much like with soy (which we will discuss next), cruciferous vegetables have been found to have a higher risk factor of thyroid dysfunction in those with insufficient iodine levels.
While soy (edamame, tofu, dairy alternatives, gluten-free products, etc.) has long been used for its estrogenic qualities to alleviate menopausal symptoms, it may be putting you at risk of developing hypothyroidism.
Soy is a well-known goitrogenic, containing isoflavones that inhibit thyroid peroxidase and iodine absorption of the thyroid gland. Genistein is the primary isoflavone found in soy, irreversibly inhibiting both TPO-catalyzed iodination and coupling. In addition, soy has been shown to decrease T4 absorption, increasing rates of autoimmune thyroiditis.
In the 1960s, a study found that infants primarily fed a soy-based formula were twice as likely to develop autoimmune thyroiditis (Hashimoto’s or Grave’s Disease) as a teenager.
Soy has been shown to work synergistically with iodine deficiency in the development of thyroid dysfunction. An iodine-insufficient diet may be required for the development of the following goitrogenic effects of soy: increased risk of goiter development, increased TSH, decreased T4, and possibly even cancer.
What? I thought we were avoiding foods that inhibited iodine absorption? Well, while iodine is essential for the production of thyroid hormones, it may be toxic in excess, potentially causing hyper or hypothyroidism. Iodine excess is most typically a result of excessive iodine supplementation rather than nutritional iodine intake.
Excess iodine levels are associated with both hypo and hyperthyroidism. Hyperthyroidism occurs as a result of the Jod-Basedow phenomenon regarding excess iodine in individuals with previously iodine-deficient levels.
Iodine-induced hyperthyroidism may be permanent or may resolve with time depending on the individual. In other cases, iodine excess has been associated with lower serum thyroid hormone levels and increased serum TSH.

Now that you know what to avoid… we can switch gears and talk about the foods and nutrients you should make sure you are getting enough of! That’s because even though “diet” invokes thoughts of restricting and cutting out, proper diets should also include healthy and important additions as well.
This will likely be exciting for people who were worried about having to cut down on their meat consumption. Foods rich in iron like liver, red meat, seafood, poultry, beans, lentils, kidney beans, cashews, and fortified foods are excellent additions to a hypothyroidism patient’s diet.
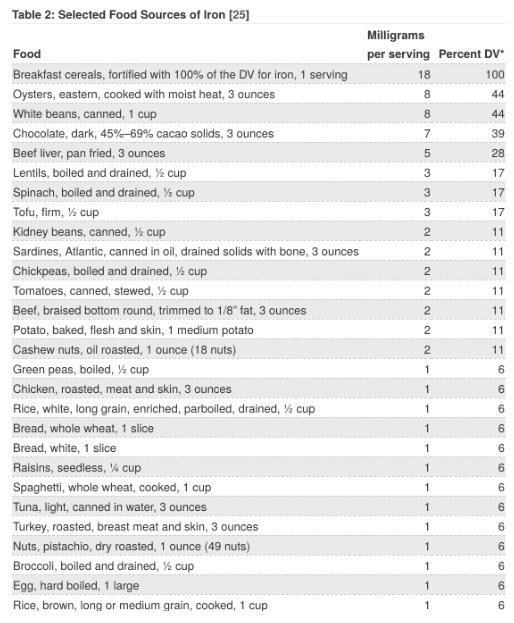
Over 2 billion people worldwide suffer from iron deficiency. The vast majority of these patients are young adult women with heavy menstrual flows. A multitude of studies have shown that iron deficiency anemia directly impairs thyroid function, resulting in a decrease in TSH production, TPO activity, lower T3 and T4 production, lower peripheral T4 conversion to T3, and increased conversion to RT3.
Not only is the body decreasing output of thyroid hormones, bost also down-regulating thyroid hormone potency by increasing symptoms of hypothyroidism.
One nutrient you may be less familiar with that is also incredibly important is selenium. Food sources of selenium include brazil nuts, seafood (yellow tuna, halibut, sardines), meat, poultry, and dairy products.
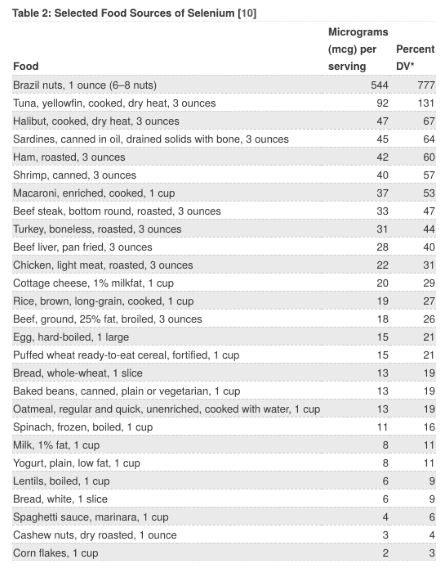
Selenium is a micronutrient and antioxidant that can be found in high quantities in the thyroid gland. Its antioxidant effects serve an important role by removing oxygen-free radicals formed throughout the process of producing thyroid hormones.
In selenium deficiency, this antioxidant effect is diminished, resulting in buildup of oxygen-free radicals, hydrogen peroxide causing thyrocyte damage, and (over time) fibrosis.
Selenium deficiency increases the risk of developing thyroid dysfunction by inhibiting thyroid hormone production and diminishing the conversion of T4 to T3. Due to this decreased production of thyroid hormones, TSH rises. Low serum selenium levels are also associated with an increased risk of developing an enlarged or nodular thyroid.
In Hashimoto’s thyroiditis, selenium supplementation of 100-200ug per day has been shown to decrease antibody levels by 40-55.5% with some participants showing complete normalization of antibody levels.
In Grave’s Disease, patients taking methimazole return to a euthyrodic state faster when supplementing selenium and other antioxidants. In addition, selenium may improve symptoms related to orbitopathy in Grave’s Disease.
Similar to iodine, you must be cautious when supplementing selenium to avoid selenium toxicity! A daily dose of 200-400mcg is considered safe, but it’s always best to be in contact with your naturopathic physician to know what is best for you.
Jumping right back to iodine, it is important to remember how we noted that while excessive iodine can have an adverse effect, having a substantial amount in your natural diet can do wonders for your symptoms. Iodine-rich foods include iodized salt, seaweed, fish (cod, tuna), shrimp, dairy, and eggs.
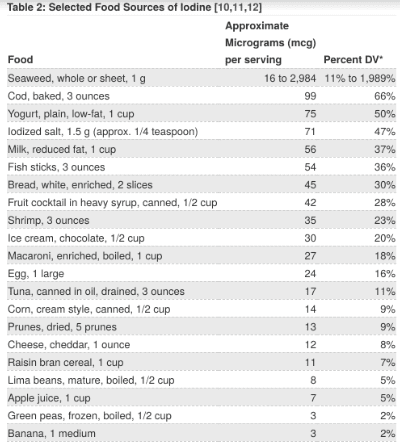
Iodine is a trace element that is naturally present in the above-mentioned foods. Iodine is an essential precursor in the production of thyroid hormones. Therefore, a diet sufficient in iodine is necessary for optimal thyroid functioning. This being said, it is important to avoid taking it in excess as it can also lead to thyroid dysfunction.
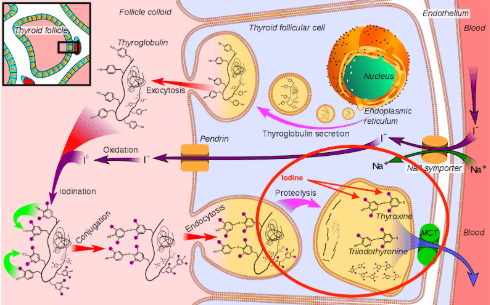
Iodine deficiency stimulates an increased production of TSH, causing an increased thyroidal iodine uptake to prevent a decrease in thyroid hormone production. As iodine deficiency progresses and becomes more severe, thyroid hormone production is unable to be preserved and will begin to fall. Typically, iodine deficiency will present with an enlarged thyroid gland (goiter).

Iodine deficiency in pregnancy and infancy is the most common preventable cause of mental retardation. Iodine deficiency during this time often results in irreversible growth and mental development disorder.
Although fruits and vegetables contain iodine, quantities vary greatly due to differences in soil quality across the world. Salt iodization programs in more than 70 countries have dramatically decreased the prevalence of iodine deficiency worldwide. Iodine insufficiency is still common in Africa, Southeast Asia, and Eastern Mediterranean cultures.
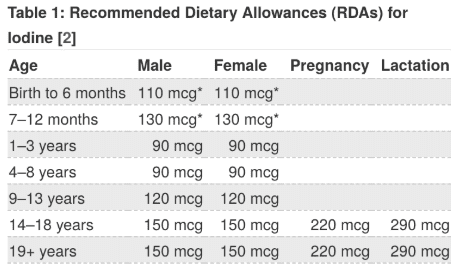
To prevent iodine deficiency, it is important to ingest 100mcg/day, although optimal iodine levels may be achieved when ingesting 250mcg-1gram per day.
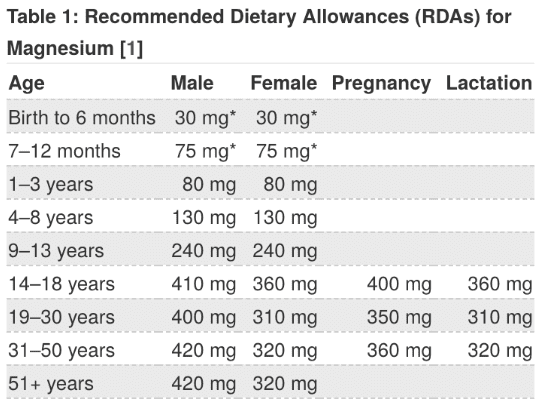
Also important is magnesium. Magnesium food sources include legumes, nuts, seeds, whole grains, leafy greens, dairy products, and fortified food products.
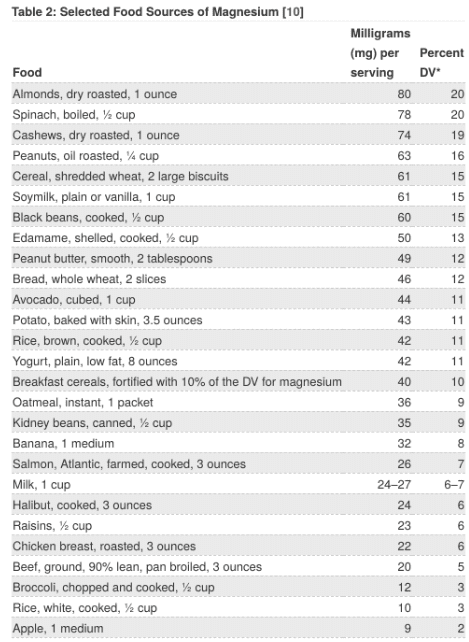
48% of the American population consumes less than the daily recommended amount which ranges from 310-420mg per day. Serum magnesium testings are not a reliable measure to rule out deficiency, however. Magnesium deficiency has been primarily linked to an increased risk of developing Hashimoto’s and increased thyroglobulin antibodies.
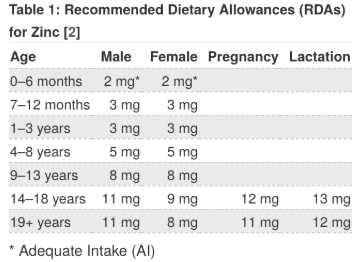
Moving onto zinc, excellent food sources include oysters, red meat, poultry, seafood, beans, nuts, dairy, and fortified food.
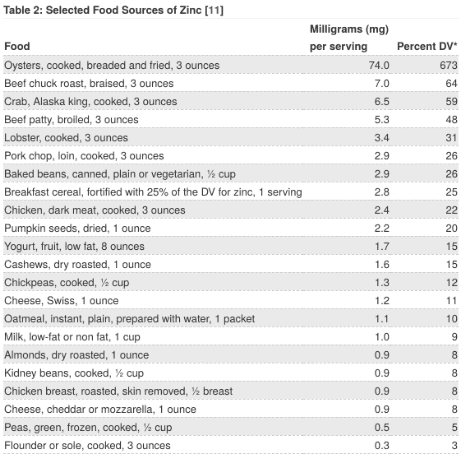
Zinc is essential for activation of the T3 receptor. Zinc deficiency decreases receptor activation and, therefore, may contribute to symptoms of hypothyroidism.
Conversely, hypothyroidism decreases zinc absorption from the GI tract which may further contribute to a low serum zinc level. Zinc deficiency should be considered a cause of subclinical hypothyroidism.
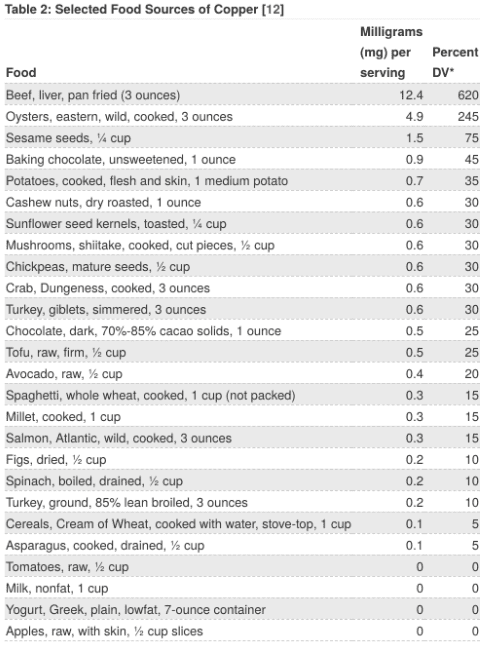
Copper-rich foods include oysters, sesame seeds, nuts, beef, liver, and chocolate.
Serum zinc concentrations are finely balanced with serum copper concentrations. Therefore, long-term zinc supplementation is often not advised due to the risk of disrupting this balance. In addition, zinc and copper compete for absorption in the GI tract. This means having high concentrations of either mineral may cause disruption to the balance.
It is estimated that around 17% of the world population has inadequate zinc intake. Harvard reports that the daily recommended intake of zinc is 11mg for men and 8mg for women. The National Health Institute considers 4-40mg of zinc safe for short-term dosing.
Hopefully this guide has been illuminating in terms of how you should be approaching your diet and lifestyle when living with hypothyroidism! It is a frustrating condition with plenty of unwanted symptoms, but it is definitely manageable when you tackle it head-on.
To recap, the areas that we discussed were:
And just like that, you’re on your way to a more energizing and fulfilling lifestyle, thyroid dysfunction or not! Did you have any other tips or tricks (or delicious recipes) that help incorporate the changes mentioned? Any other specific questions about what you should be doing? Feel free to reach out and we can get started on changing your life together!
Hello, my name is Dr. Sarah Bennett, NMD!
I am a naturopathic physician licensed in the state of Arizona currently practicing at my office in Scottsdale, AZ. I received my degree from Southwest College of Naturopathic Medicine, did a year residency at Keystone Natural Family medicine, and received additional training for aesthetics & anti-aging at National Laser Institute.
My passion and fascination for natural medicine began during my undergraduate studies at Indiana University where I got a dual degree in neuroscience & psychology.
I saw how a preventative approach could help you live a long and youthful life. Since then I have dedicated my life to serving others to understand the latest medical trends.
I spend my spare time running, hiking, rock climbing, camping, testing out new diets, and reading books on latest medical trends / listening to podcasts to find the latest nuggets of knowledge to improve the quality of life for my patients. I look forward to serving you!