By Dr. Sarah Bennett, NMD / August 15, 2020
Over 50% of the adult american population is diagnosed with prediabetes or diabetes.
This means that there are more sick than healthy people in America due to diabetes alone!
Since the 1980s, just one generation, rates of type 2 diabetes have risen by an astonishing 1160 percent! In 2014, 422 million people worldwide suffered with type two diabetes, and prevalence continues to rise. (1)
This is likely why the production of anti-diabetic medication has risen at an exponential rate. Between 2004 to 2013 alone, 30 new anti-diabetic medications were brought to market. (1)
Yes, research and development is needed to improve the medications and management of type 2 diabetes. And yes, these medications greatly improve management of blood glucose levels in millions of people world wide.
But don’t be fooled! These medications are also one of Big Pharma’s top money makers, with sales of diabetes medications reaching $23 billion dollars by 2015. Lantus (a long acting form of insulin) alone brought in $7.6 billion in 2013. (1)
And to top it off, there have been steep price increases for these medications. Especially the newer insulins, having prices that rose between 168 to 325 percent from 2010 to 2015 alone.(1)
Excuse me if I come across cynical, but I find this completely absurd.
Our government subsidizes the food that is shown to highly contribute to the development of type 2 diabetes, making these foods most accessible and affordable by the majority of our population. And then the health care system profiteers off of the medication created to manage this disease.(1)
Please don’t misunderstand me.
Medications are beneficial and often necessary for the treatment of many conditions, but don’t just take the advice of your medical practitioner.
I wholeheartedly believe that it is essential for each person to educate themselves about their individual healthcare needs.
Throughout this article, I will review the conventional medications, insulins, surgeries, and devices used to manage type diabetes.
It is my goal to provide you with the necessary information needed to make educated decisions about your own medical care.

As a quick review, type 2 diabetes is a chronic condition that progressively develops over many years, due to diet, lifestyle, and genetic factors. It is characterized by consistently, abnormally elevated blood glucose levels.
For more detailed information about type 2 diabetes read my comprehensive article.

Simple blood tests are able to measure insulin, and blood glucose control, which are used to evaluate diabetes risk and diagnosis.
Prevention and early detection is the name of the game!
Remember that in any disease, prevention is always better than cure. And the only way to ensure prevention of diabetes is through completing regular blood tests.
The American Diabetes Association’s diagnostic criteria for diabetes are the following: (2)
OR
OR
OR
If you have not checked these numbers recently or are concerned that you may have diabetes ask your naturopathic physician for a comprehensive workup.
The American Diabetes Association recommends regulation of blood glucose, cholesterol, and blood pressure for optimal management of diabetes. Blood glucose and HbA1c targets are dependent on the severity and duration of diabetes, as well as the presence of comorbid conditions, and life expectancy. (3)
Mild cases of diabetes will strive to achieve complete correction of HbA1c, <6.5%, yet a more reasonable goal for the majority of patients is <7.0%. Oftentimes an HbA1c is difficult to achieve while avoiding hypoglycemia and other adverse effects. Patients with long standing diabetes may set the goal even higher, at <8.0%, due to the presence of other comorbid conditions, complications, and shorter life expectancy. (3)
Similar to HbA1c, the goal for fasting blood glucose will vary between 80-130 mg/dl depending on the severity of diabetes. (3)
Although the epidemic of diabetes type 2 started in the 1980s, the disease was first documented in Ancient Egypt around 1550 BC. This is not a new disease! And despite this fact, diabetes type 2 is fundamentally misunderstood, and improperly treated.
Type 2 diabetes is primarily a disease of lifestyle and dietary origin, yet conventional treatments consist of medications, devices, and surgical procedures rather than nutritional and lifestyle reform. This is likely due to the fact most medical associations today are funded by pharmaceutical and medical device companies.
These conventional treatments primarily aim to reduce blood glucose, but neglect the progressively elevating insulin levels. Anti-diabetic medication effectively lowers blood glucose (temporarily) but ultimately fails to cure the disease.
To be fair, these medications, devices, and surgical procedures are currently essential therapies used to manage diabetes in millions of people world wide. They do help control blood glucose levels, and even save lives. The problem is, the majority of these therapies do not cure the disease of or even start to reverse the progression, and often have side effects such as significant weight gain.
When it comes to any disease it is important to understand all treatment options available, enabling you to make an educated decision on how to proceed with your own choice in therapy. Below I have listed the most common conventional medications used to treat type 2 diabetes.

Below I review the most common oral antidiabetic medications prescribed for management of diabetes:
Metformin is the recommended first line medication for diabetes, and may be dosed alone or in combination with sulfonylureas such as glipizide or even with DPP4 inhibitors or sitagliptin.
Metformin works to improve insulin sensitivity, decrease the production of glucose from the liver, and decrease the absorption of glucose in the gastrointestinal system.
It is the one of the only antidiabetic medications that does not have the side effect of significant weight gain, due to the fact it does not raise insulin.
In addition, many physicians are beginning to prescribe this medication for its anti-aging and preventive effects. Metformin not only aids in weight loss, but has also been shown to help prevent cancer, atherosclerosis, stroke, atrial fibrillation, neurodegenerative diseases, and even prolong life span. (5)
The most common side effects of metformin are related to the stomach like nausea and vomiting, abdominal bloating, heartburn, and constipation. Since Metformin is eliminated through the kidneys, it is unsafe for patients with increased creatinine and those with kidney injury or damage.
Sulfonylureas, such as Glipizide lower blood glucose by stimulating an increased secretion of insulin from the pancreas, decreasing the rate of hepatic glucose production, and increasing the sensitivity of the insulin receptor in peripheral cells.
Sulfonylureas were discovered in 1942 and have since been widely used for the management of diabetes.
These medications tend to be cheaper but due to increasing insulin production come with a high risk of hypoglycemia and substantial weight gain. The risk of hypoglycemia is even more significant in the elderly, malnourished, and in those that have an infection, trauma, or surgery.
Research has shown little to no benefits in prevention of long term diabetic complications, and only mild cardiovascular benefits due to the significant increase in weight gain after beginning these medications. (1)
Patients with liver or kidney dysfunction are not advised to take this medication due to being metabolized through the liver and eliminated through the kidneys. In addition, it is not advised that this medication be taken by the elderly and those with alcoholism. (6)
Thiazolidinediones such as rosiglitazone, have been banned in Europe since 2010 for the determination that the overall risks of taking the medication outweigh the benefits.
Thiazolidinediones decrease blood glucose levels by increasing insulin sensitivity in adipose (fat), muscle, and liver cells, increasing glucose utilization in these cells and decreasing glucose production. (6)
Due to increasing insulin sensitivity in fat cells, significant weight gain can be expected. On average a patient can expect to gain 6.6 to 8.8 pounds of fat after beginning treatment. (1)
These medications have an efficacy similar to that of metformin, yet even in the United States they are considered third line therapy and less likely to be prescribed based on their high cost and adverse effects.
In addition to weight gain, patients taking Thiazolidinediones experience a significant increase in appetite and fluid retention. This fluid retention often accumulates around the ankles, but may occur in the lungs, increasing risk of congestive heart failure.
In addition, these medications increase risk of fracture due to decreasing bone density, and severe liver damage. It is important that liver enzymes are monitored at the start of treatment and every month for 12 months thereafter to make sure the liver is working optimally.
SGLT 2 inhibitors are the newest class of anti diabetic medications, usually used for patients with high risk for morbidity and mortality, since these medications are considered to be more protective against cardiovascular disease.
SGLT 2 inhibitors reduce the reabsorption in glucose through the kidneys, increasing its urinary excretion. Since the mechanism of action is independent of insulin activity, there are lower risks of hypoglycemia, fatigue, and over stimulation of the beta cells of the pancreas. In addition, patients often experience weight loss. (6)
Although, SGLT inhibitor medications have only mild effects on lowering blood glucose, they have been shown to significantly decrease risk of mortality by 38%, risk of kidney disease by 40%, and risk of dialysis by 55%. (1)
And there is more good news! The common side effects of SGLT inhibitors are generally mild and treatable, including urinary tract infection, yeast infection, genital infection, upper respiratory tract infection, dyslipidemia, and nausea.
Alpha-glucosidase inhibitors, such as Acarbose have been used to treat type 2 diabetes for over 20 years.
Alpha-glucosidase inhibitors act to inhibit the metabolism of carbohydrates in the GI tract, resulting in delayed carbohydrate digestion and absorption. This disruption in carbohydrate metabolism results in lower blood glucose following meals.
Although they have modest effects on long term blood glucose control, they also have lower risk of hypoglycemia, and do not cause weight gain.
Common side effects include abdominal pain, diarrhea, flatulence, and elevated liver enzymes. Side effects can be significant often leading to discontinuation of the medication. Due to the side effects, alpha-glucosidase inhibitors are contraindicated in patients with chronic and severe digestive disorders.
Fulminant hepatitis is a less common but fatal side effect noted in post-marketing reports of acarbose. Patients usually present with jaundice, hepatitis, rash, skin redness, and decreased platelet count. (6)
DPP 4 inhibitor’s act to prolong and elevate the activity of incretin, a hormone that increases the release of insulin and reduces the secretion of glucagon.
These medications are considered very safe, with low risk of developing hypoglycemia, and other adverse effects. Risk of weight gain is low since the elevation in insulin is not sustained. Common side effects of these drugs include headache, sinus infection, upper respiratory infections, diarrhea, and nausea. In addition, patients taking sitagliptin should be wary of the adverse effects of muscle break down, headaches, and muscle pain. (6)
DPP 4 inhibitors are eliminated through the kidneys and for safety precautions, doses should be modified in patients with renal and hepatic impairments.
GLP 1 receptor agonists like dulaglutide are injectable medications, and therefore are generally prescribed as third line therapy for treatment of diabetes.
These medications are peptides that resemble GLP-1 incretins in the body. These incretins (and therefore GLP 1 receptor agonists) act to increase insulin secretion, decrease glucagon secretion, slow gastric emptying, and decrease appetite.
Weight loss is often experienced due to the slowing of gastric emptying and resulting decrease in appetite and food consumption. (1)
Common side effects include nausea, increased amylase, and lipase (both are pancreatic hormones), diarrhea, vomiting, and abdominal pain. They are associated with a mild risk of developing hypoglycemia, unless given with other medications that will enhance this effect, such as sulfonylureas.
In addition, these medications are not recommended in patients with a personal history of pancreatitis, diabetic retinopathy, and family history of medullary thyroid cancer.
GLP-1 receptor agonists are reported to reduce the cardiovascular risk and there is no need for dose adjustment in patients with kidney disease. (6)
Meglitinides, similar to sulfonylureas are considered insulin secretagogues. They stimulate the beta cells of the pancreas to secretion of insulin by block channels of ATP in the body.
Due to these medications’ effect on insulin secretion, there is a high risk of hypoglycemia and significant weight gain. In addition, common side effects include upper respiratory tract infection, headaches, and loss of efficacy due to pancreatic beta cell burnout.
Metabolism and elimination of these drugs is through the liver and GI tract, and therefore there is no need for dose adjustment in kidney disease. (6)

When blood glucose levels fail to be controlled by our own insulin production and the antidiabetic medications listed above, insulin is prescribed.
Insulin therapy is typically administered via injection under the skin throughout the day to help control blood glucose levels. Taking exogenous insulin helps to raise insulin levels even higher to overcome the body’s significant insulin resistance, forcing cells to take up glucose in hopes of minimizing organ damage.
Patients often dread beginning insulin therapy, due to its adverse effects of rapid weight gain, high risk of hypoglycemia, and oftentimes life long dosing via daily injections.
This being said, Insulin therapy is often essential for proper management of blood glucose levels once diabetes has progressed significantly.
There are various types of insulin, often prescribed in combination for optimal glucose management. These types are listed and discussed below.
Three characteristics differentiate each type of insulins:
There are now six main types of insulin available in the market: (7)
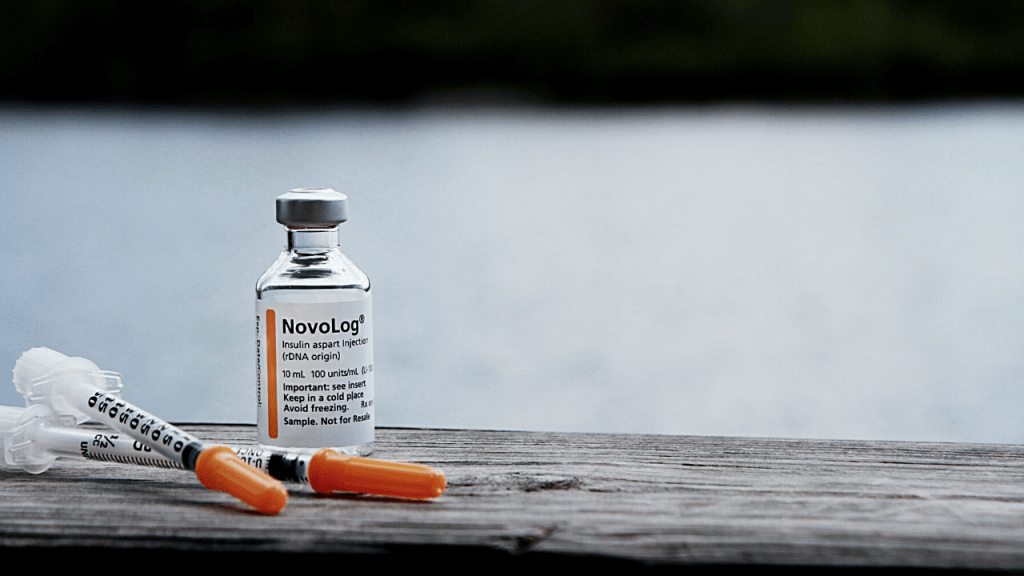
The onset of this type of insulin is less than 15 minutes and peaks within 30 to 90 minutes. The duration is estimated to last 2 to 4 hours.
Commonly used brands are Apidra, Humalog, and Novolog.
Not only can rapid acting insulin stabilize post-meal blood sugar, but it is used to to treat high blood glucose resulting from medications like steroids, antibiotics (especially fluoroquinolones) and acute infections.
On the other hand, rapid acting insulin has a high risk of hypoglycemia ( low blood sugar) and hypokalemia (low blood potassium). Hypokalemia is the result of elevated Insulin shifting potassium into the cell and thus out of the blood stream.
2. Short or regular acting Insulin, similar to rapid acting insulin, are also used to lower post-meal blood sugar.
This type of insulin has an onset of 30 minutes, will peak in 2 to 4 hours, and has a duration of 3 to 6 hours. Humulin R and Novolin are common brands of regular insulins.
Regular insulins also have a high risk of causing hypoglycemia, but due to acting over a longer duration hypoglycemia may occur 3 to 4 hours after administration. This prolonged time between dose and possible hypoglycemic attack, may increase difficulty of finding the appropriate dose.
In addition, regular insulins commonly cause diabetic retinopathy, hypokalemia, and weight gain. (8)
One major advantage of regular acting insulin is that it can be used through intravenous administration to treat diabetic ketoacidosis or severe hyperglycemia due to predictable and stable effects.
3. Intermittent or Intermediate acting Insulin is prescribed as a “longer” acting insulin to stabilize blood glucose levels over half a day.
This type of insulin has an onset of 2 to 4 hours, peaking at 4 to 12 hours, and having a duration of roughly 12 to 18 hours. Humulin N and Novolin N are common brands.
Although less than regular or rapid acting insulin, intermediate acting insulins have a high risk of hypoglycemia, hypokalemia, and weight gain. Intermediate acting insulin has a lower risk of hypoglycemia due to having a longer duration and lower peak.
4. Long-Acting Insulins are injected once daily and used to stabilize insulin over a 24 hour period of time. The onset of this type of insulin is 6 hours, does not peak, and has a duration of 24 hours. Levemir and Lantus are common brands.
Due to having no peak and even longer duration, long-acting insulins have an even lower risk of hypoglycemia. This being said, if a larger than normal meal is eaten, this type of insulin may fail at regulating post-meal blood glucose. Long-acting insulin will also cause hypokalemia and weight gain.
5. Ultra long-acting Insulin, like long-acting insulin, is injected once daily and used for consistent stabilization of blood glucose over a long period of time.
The onset of this type of insulin is 6 hours, with no peak, and a duration of up to 42 hours. Toujeo is a common brand of ultra long-acting insulin.
Ultra long-acting insulin can be used for better glycemic control with very low risk of getting hypoglycemia. Like long-acting insulin, it may not be able to blood glucose levels after eating a large meal. And don’t forget, this type of insulin may also cause hypokalemia and weight gain.
Comorbidity describes two or more disorders or illnesses happening in the same person. Patients with type 2 diabetes may have other illnesses like hypertension, increased cholesterol, heart problems, and kidney problems. Below we discuss some of the common medications that may be given when you have these comorbidities:
Patients commonly have elevated cholesterol secondary to diabetes, further increasing risk of cardiovascular disease. Statins and fibrates are both used to lower “bad cholesterol, triglycerides, LDLs, and VLDLs.
Common side effects of these medications are mild muscle pain, headaches, dizziness, nausea, diarrhea, and bloating.
While statin medications block the production of cholesterol, they also block production of the essential antioxidant CoQ10 in the body, oftentimes causing deficiency and associated symptoms. CoQ10 deficiency presents with muscle stiffness and spasme, vision loss, hearing loss, eye twitching, and neurological dysfunction, such as seizures, and cognitive decline. This associated deficiency oftentimes contributes to the muscle pain commonly seen as a statin side effect. If you are currently taking a statin be sure to supplement CoQ10 to avoid deficiency and these unwanted symptoms.(9)
Although mild muscle pain is a common side effect, occasionally patients will experience severe muscle pain, causing a serious adverse effect called rhabdomyolysis, or the painful breakdown of muscle tissue. The higher the dose of statins, the higher the risk for rhabdomyolysis, and although supplementation of CoQ10 may mildly help with symptoms, it does not resolve the muscle breakdown.
Because statins are cleared through the liver, these medications may raise liver enzymes, and rarely cause liver damage. After starting a statin medication be sure to have your liver enzymes checked at least 12 months post initiation.
Aspirin is a NSAID ( nonsteroidal anti-inflammatory drug) used for its blood thinning effects in diabetic patients with high cardiovascular risk. A daily dose is typically recommended to patients who have had previous heart attacks and strokes.
Be aware that NSAIDs notoriously cause GI upset and kidney damage when taken frequently and in high doses. Aspirin is contraindicated in patients with bleeding disorders, and conditions that increase risk of bleeding such as alcoholism and peptic ulcers.
Common side effects are abdominal pain, vomiting and bleeding.
ACE inhibitors such as Lisinopril are most commonly used to lower blood pressure. In diabetic patients these medications are frequently prescribed even in absence of elevated blood pressure for their kidney protective effects.
On the other hand, in cases of acute kidney injury, lisinopril is not recommended because it decreases the filtration rate of the kidney.

Bariatric Surgery is a broad category of procedures used to treat obesity and diabetes. These procedures on the stomach and small bowel restrict food intake, decrease absorption, and alter hormone production.
The various types of procedures are categorized by two characteristics.
The 3 most popular of these procedures are listed below:
The Roux-En-Y bypass is a modern blocking and restrictive procedure used to treat more severe cases of obesity due to having a high risk of complications.
This procedure removes a large portion of the stomach shrinking it to the size of a walnut and reroutes the small intestines to create a Y shape.
The Roux-En-Y bypass procedure results in the best weight loss in comparison to other procedures, Although it does come with the most complications.
In addition to complications common to all procedures, bleeding and infections, the Roux-En-Y bypass often commonly results in nausea, diarrhea, facial flushing, strictures, multiple nutrient deficiencies and life-long malnutrition. (10)
The gastric sleeve is a restrictive procedure that removes a large portion of the stomach without removing or changing any portion of the small intestines.
Although, after surgery no more than a few bites of food are able to be eaten at a single meal, over time the stomach will stretch a portion size equivalent to a small meal.
Due to being a laparoscopic procedure, the gastric sleeve surgery has less complications than the Roux-En-Y bypass. Most commonly, patient experience gastric dumping, strictures, nausea, and vomiting.
Overall, this procedure yield less weight loss which generally rebounds in a shorter period of time.
The gastric lap band surgery is the simplest restrictive procedure.
This procedure does not remove or alter any part of the stomach or small intestine. Instead, an adjustable band is placed around the stomach to restrict the ability of food to enter the stomach.
The weight initially lost is commonly regained over time, leading to patients having the lap bands removed.
Bariatric surgery has been shown to consistently result in weight loss and rapidly reverse diabetes.
These procedures have shown such great success that 45 diabetes organizations, including American Diabetes Association have recommended bariatric surgery as a first-line treatment option for diabetic patients with a BMI greater than 40, regardless of lifestyle intervention. (11)
Despite consistent results, these procedures are much less common that oral and injectable medication due to the high cost.
Although longevity of results are generally not maintained with exception of the more complicated surgeries such as the Roux-En-Y bypass, these surgeries teach us that diabetes is reversible, and rapidly reversible at that. Correction in blood glucose levels is typically seen within weeks of surgery.
So now many of you are probably thinking “Alright! Sign me up.”
Well, what if I told you that you can likely get these results without major surgery? Yes, that’s right.
The consistent weight loss and diabetes reversal seen across procedures is most highly due to sudden severe calorie restriction, rather than hormonal changes. (11)
The good news is that this can be accomplished with simple fasting protocols!
For proper management of blood glucose in diabetes it is important that patients monitor their glucose levels frequently. Lancets and Glucometers make self monitoring of blood glucose levels easy and accurate.
Glucometers or blood sugar meters are the most common device used for at home blood sugar checks.
When using blood sugar meters, you first need to wash your hands thoroughly. Prepare an alcohol swab and dry cotton to use when pricking your finger, next, insert a blood glucose meter, afterward, you can have somebody assist you in pricking the tip of your finger (or you can do this yourself), then carefully place a drop of blood in the meter and wait for the blood glucose reading to appear.
The cost of blood sugar meters will vary depending on the model and the strips needed to use them. Insurance companies will often cover certain devices, so check which device is covered under your plan!
As technology improves, newer and easier to use meters have become more available. Some newer metes come with illuminated and bigger screens, large easy to use buttons, and even a save option to see previous results.
With the numerous glucometers for sale it can be difficult to determine which option is best for you. Below, I have listed 3 of the most popular glucometers to aid you in your search.
1. Contour NEXT EZ Glucometer

It’s fast, accurate and can give your results in just five seconds. No coding or calibration is required when you get new test strips, making it easy to use. This device provides an alarm to schedule and remind you of blood sugar monitoring times. And lastly, it can save all your results!
It is available at https://www.contournextstore.com/en/blood-glucose-meters at $19.99.
2. AccuCheck Aviva Plus

Accu-Chek Aviva Plus is known for its accuracy. It has a 150 system integrity check which detects unreliable results, making sure that your blood glucose level will always be accurate and precise, making your diabetes more manageable. The device also uses less blood and is proven to be less painful than other brands in the market.
It is available on Amazon (https://www.amazon.com/Accu-Chek-Aviva-Glucose-Monitoring-System/dp/B07DRMT15K/ref=pd_sbs_121_3/137-3628426-8299511?_encoding=UTF8&pd_rd_i=B07DRMT15K&pd_rd_r=17b76aad-52b1-4b81-8315-ef920a88d910&pd_rd_w=xiJS5&pd_rd_wg=fTqvX&pf_rd_p=bc074051-81d1-4874-a3fd-fd0c867ce3b4&pf_rd_r=NEF0NDRNZHP3BDMJ7AW1&psc=1&refRID=NEF0NDRNZHP3BDMJ7AW1) at $32.79.
3. Prodigy Glucose Monitoring

The prodigy glucose monitor is perfect if you are visually impaired since it can guide you through the process and read your result out loud.It even comes in several languages like English, Arabic, French and Spanish.
It is available on Amazon at $18. (https://www.amazon.com/Prodigy-Glucose-Monitor-Kit-Carrying/dp/B07S2T64BL/ref=sr_1_3?dchild=1&keywords=Prodigy+Glucose+Monitoring&qid=1596072575&s=hpc&sr=1-3)
Lancing Devices and Test Strips are used together with a glucometer. It is important to take note that lancing devices are only used once and discarded immediately.The type of test strips needed will vary depending on brand and model of glucometer.
Below, we have listed 3 of the most popular lancing device on the market:
1. Genteel Lancing Device

Pros: It has six depth levels available and the lancet is almost pain-free! A vacuum pump is included to help the blood flow better on the tip of the finger.
Cons: It is expensive in comparison to other lancing devices and is easier to use on others than self.
The Genteel lancing Device can be purchased at https://www.mygenteel.com/products/genteel It for $49.99.
2. Fastclix Accu-Chek Fastclix Lancing Device

Pros: It has a barrel that contains six lancets, no need to reload every time you check your blood sugar!
Cons: It has a multiple click lancet that may be difficult to use for first timers.
The Fastclix Accu-Chek Fastclix Lancing Device may be purchased at https://www.accu-chek.com/lancing/fastclix-lancing-device for $23.99.
3. Care Touch’s Adjustable Lancing Device

Pros: It has 10 depth levels available and lets the user find their preferred lancet depth. The barrel is also made longer, thus making it easier to use.
Cons: The lighter depth levels cannot easily break the skin. The user may need to do some trial and error before finding the perfect depth.
The Care Touch’s Adjustable Lancing Device can be purchased at https://www.caretouchusa.com/product/lancing-device-with-ejector/ for $7.99.
Other High Tech Devices

Continuous Glucose Testing Monitors
With the advancement of technology, newer and better devices have been made to make blood testing easier and more comfortable for patients.
Continuous glucose testing monitors include a sensor that is placed under your skin to continuously monitor blood glucose levels.
A recording device or microchip is worn so that it can connect to a smartphone or a smartwatch. It allows you to set your phone or watch to alarm when blood glucose readings are too high or low.
Advantages:
Disadvantages:
The diagnosis of type 2 diabetes can be overwhelming, much less trying to understand and manage the medications and treatments for this condition.
It is my goal to provide you with all the important information about the most common conventional treatments for diabetes, how they work, how they help, and what to be cautious of.
Take your health into your own hands! Use the information in this article to work alongside your medical practitioner in creating a personalized treatment plan for your specific needs.
Be sure to include the simple but powerful natural treatments for optimal diabetes management and reversal. There are many researched backed supplements, dietary protocols, and lifestyle changes that can change your life.
As a recap, we have discussed the following in this article:
Table of Contents
For more information on natural treatments for diabetes read my article here.
References