By Dr. Sarah Bennett, NMD / December 12, 2019
Stress, difficulty sleeping, sluggish mornings… these are all things that can throw your entire body off its rhythm (and even make you sick). So, what is the root of it all at a physiological level?
Fortunately, you can trace a lot of this (and more) to your cortisol hormone. The less fortunate news is that it can be a little complicated. And for how important a hormone it is, this can become a significant problem in your life if imbalanced and unaddressed.
That’s why I’m here to help you understand the basics! By knowing how cortisol works with your body and what you can do to make sure it is at the right levels, you will be able to make lasting changes in your life and have more informed conversations with your doctors.
Without further ado… what is cortisol? Why does it matter? Find out everything you need to know in this ultimate guide!
The best place to start is explaining what exactly cortisol is. That way, everything else can fall into place pretty easily!
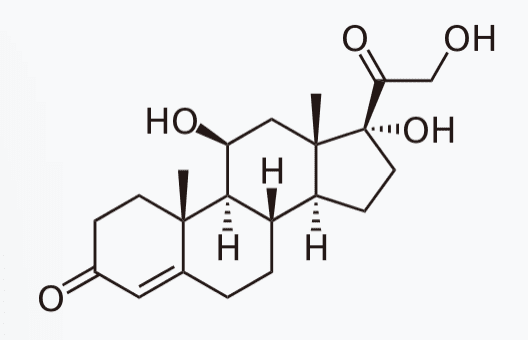
Cortisol is the body’s primary stress hormone. It is produced from the cortex of the adrenal gland, a triangular shaped organ that sits on top of the kidneys. It is a glucocorticoid, steroid hormone that is created from cholesterol through the long, enzymatic pathway shown below.
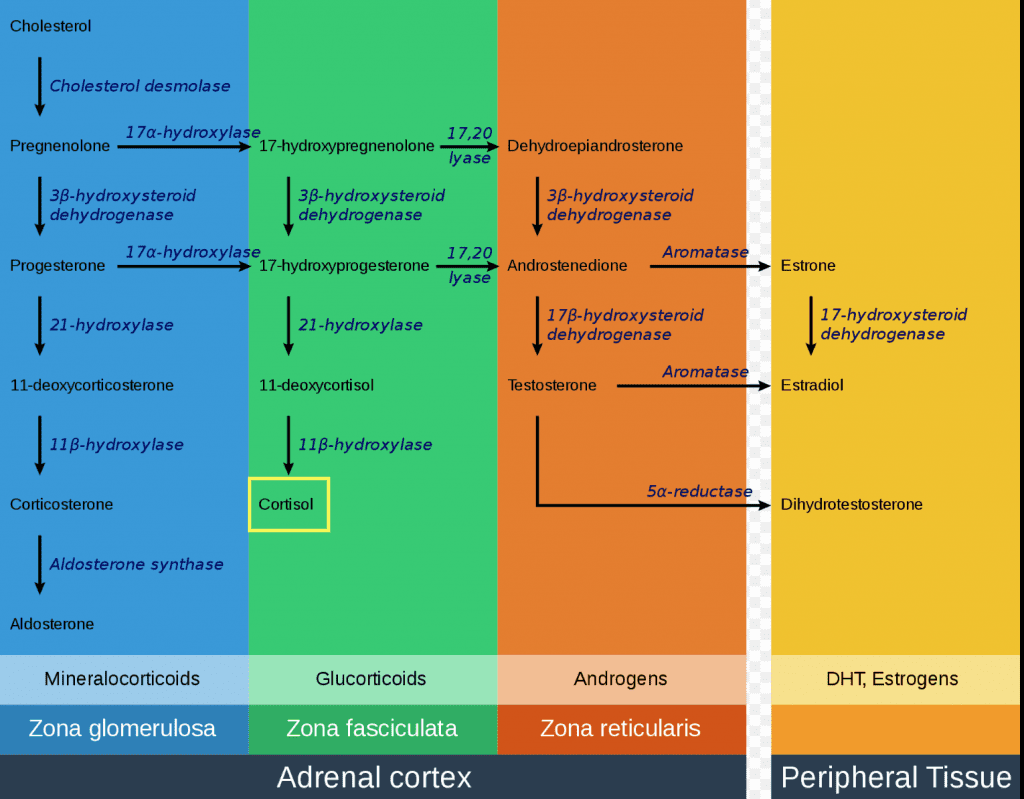
This process is very similar to that of sex hormone production.
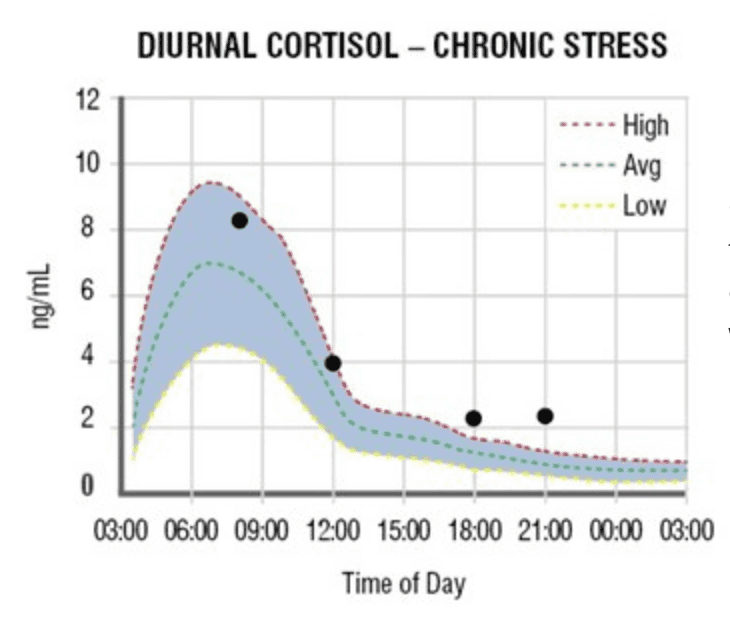
The levels of cortisol in your body naturally fluctuate throughout the day. They typically elevate in the morning around 6 a.m. to give us energy and wake us up and gradually fall throughout the day until levels reach their lowest in the evening so we can fall asleep.
This curve is ideal and healthy, yet only seen in a perfect world without daily stressors and artificial light. Since this diurnal cortisol curve is influenced by the amount of light in our environment, it can be incredibly sensitive to even seemingly mundane (and unavoidable) things like having your lights on after dark. The levels are designed to elevate with sunrise and decrease with sunset, playing a big part in our circadian rhythm (sleep wake cycle).
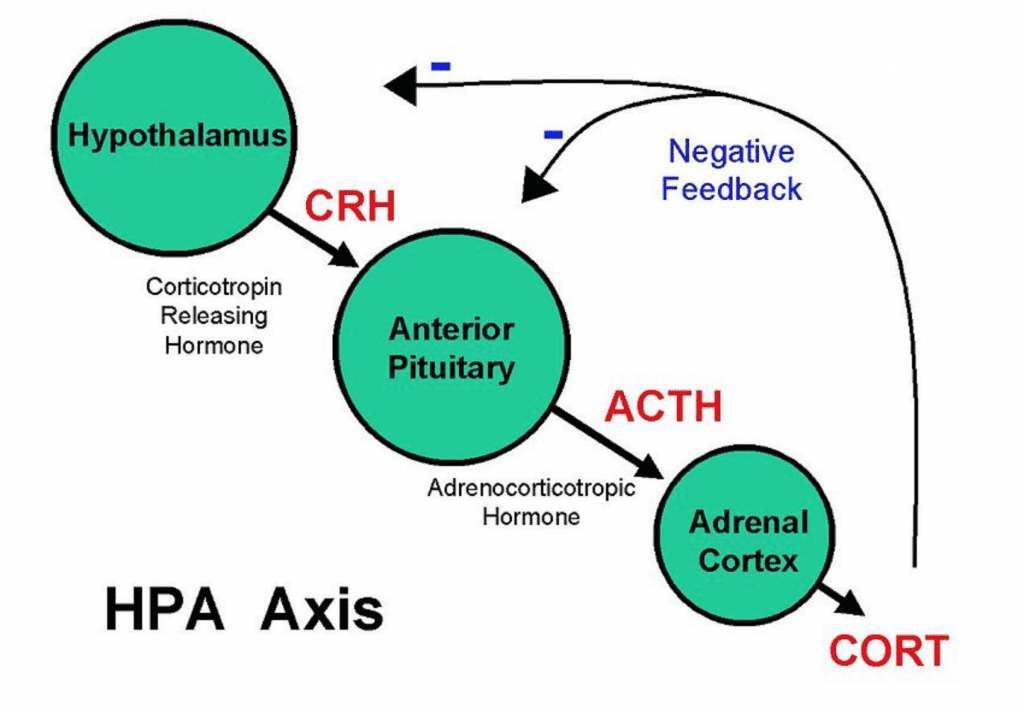
The secretion of cortisol is controlled by the HPA axis. This includes the hypothalamus, pituitary gland, and adrenal gland. For hours after a stressor, the hypothalamus will produce Corticotropin (CRH). This releases the hormones that will travel through the bloodstream and bind receptors in the pituitary.
In response, the pituitary will produce adrenocorticotropic hormones (ACTH) to signal that it is time for the adrenal glands to produce cortisol. This will elevate cortisol in response to a stressor that causes enhanced alertness, change of mood that leads to anxiety or irritability, increased energy, and potentially panic or fear.
Cortisol production influences many functions of the body. This includes (but is not limited to) the body’s stress response, the circadian rhythm, blood glucose concentration and insulin sensitivity, bone formation, immune function, and body fat gain/loss.
Every cell in the body has receptors that bind cortisol. Cortisol is the body’s primary stress hormone. When elevated, it will stimulate the “fight or flight” response and shut down bodily functions that are not a top priority in a life or death situation. It is also the only hormone that rises with age.
Long-term adrenal hyperactivity will influence many other functions of the body, including:
Cortisol is a steroid hormone and, much like prednisone, it is anti-inflammatory in nature (particularly when initially elevated). For this reason, long-term stress that results in chronically elevated cortisol levels will release pro-inflammatory cytokines. This increases systemic inflammation and results in immune dysfunction.
Chronically elevated cortisol levels have been shown to decrease lymphocytic proliferation. This causes latent viruses to resurface and aggravates disease progression in things like autoimmune diseases and irritable bowel syndrome. Chronic stress may even put you at a higher risk of developing autoimmune diseases in the first place!
How does this happen? Chronic stress often leads to glucocorticoid resistance and impaired HPA responsiveness, resulting in hypocortisolism. Hypocortisolism enhances inflammation in the body and increases the risk of developing or advancing autoimmune conditions. In addition, hypocortisolism has been linked to chronic fatigue syndrome and systemic pain conditions such as fibromyalgia.

Cortisol directly counteracts insulin in the body. After eating a meal, blood glucose rises and signals the release of insulin. Insulin is released to stimulate the cells’ uptake of glucose, resulting in a decrease and normalization of blood glucose levels.
In times of stress, cortisol is released and will prevent cellular glucose uptake. This stimulates gluconeogenesis, the creation of glucose from glycogen stores in the liver and muscles. This will elevate blood glucose levels, providing the body energy to escape the stressful situation.
In cases of long-term stress, this results in consistent elevation of not only cortisol, but also blood glucose and insulin levels. Over time, cellular receptors are desensitized to insulin, thus creating insulin resistance and increasing the risk of type 2 diabetes.
Just as hypercortisolism induces insulin resistance (and type 2 diabetes over time), chronic hypocortisolism induces and elevates insulin sensitivity. This leads to decreased gluconeogenesis from the glycogen stores in our liver and muscles. Further, this creates a higher risk of hypoglycemia, which may cause lightheadedness, increased hunger, shaking, and fatigue.
Thyroid hormones help regulate the cellular metabolism. Elevated cortisol levels have been linked to clinical and subclinical hypothyroidism.
Chronically elevated cortisol is linked to clinical and subclinical hypothyroidism. This will generate weight gain and specifically increases amounts of abdominal and visceral fat. An extreme version of this is seen in Cushing Disease which results in excess abdominal fat and thin limbs in response to cortisol mobilizing fat tissue from the periphery to the abdominal region. Central adiposity and visceral fat then increase the risk of cardiovascular disease, cancer, and mortality.
Mental and emotional health are frequently overlooked and untreated, yet they are key to a satisfying and productive life. Anxiety is the most common mental illness in the United States, affecting 40 million people. Major Depressive Disorder is the leading cause of disability in the United States and affects 16.1 million adults.
Often, people suffer from these mood disorders simultaneously. Nearly 50% of individuals diagnosed with depression also suffer from anxiety.
Stress, anxiety, and cortisol levels are directly related. Cortisol will spike in times of acute stress and cause an increase in anxiety or even panic. Individuals with panic disorder are shown to have more difficulty regulating their cortisol levels post-stressor. Studies have also shown that elevated cortisol is linked to those suffering from depression or even those considered high-risk for depressive symptoms.
I commonly see that my chronically stressed patients will crave salt and experience dizziness upon standing. This is because cortisol helps to regulate blood pressure and electroylte status in the body.
Chronic hypocortisolism leads to low blood pressure and hypotension (a drop in blood pressure upon standing). This most commonly causes lightheadedness or dizziness as a result, but it can also cause nausea, confusion, and blurred vision.
Hypocortisolism will also cause imbalances in electrolytes, hyponatremia (low sodium), and hyperkalemia (elevated potassium). This explains the salt cravings! The low sodium further contributes to the low blood pressure and will worsen the symptoms listed above. Talk about a vicious cycle!
For these patients, adding salt to the diet is actually beneficial! This and other unexpected solutions to dietary problems are precisely why I recommend seeing a naturopathic doctor before making dietary and lifestyle changes based on one-size-fits-all recommendations.
Something that virtually everyone deals with at some point or another in their life is the frustrations of hormone imbalance.
In times of stress, the body will shut down functions that are not necessary for survival. High on that list is all reproductive functions, as it is more important to run from a tiger than to make a baby.
This means that chronically high stress can really throw your other hormones (especially sex hormones) out of balance and impact more areas of your life than just reproduction. We will dive deeper into how cortisol works with other hormones later, but for now, just note that imbalanced cortisol can and will lead to other hormone imbalances as well.
The immunological response to chronically elevated cortisol in response to chronic stress is associated with advanced aging.
Telomere length is a measure for physiological age. Long-term stress will result in telomere strength shortening more quickly, further resulting in a sped-up aging process.
This is something that is hard to reverse, but if you look into some of the amazing services that are offered at medical spas in addition to your naturopathic treatments, you can help to roll back the clock and get some of your youth back (both internally and externally).
As mentioned, many of the ways that cortisol impacts the body are impacted by the way it works with other hormones – this includes problems like hormone imbalances.
One example would be the way in which cortisol interacts with thyroid hormones. Since thyroid hormones help regulate the cellular metabolism, elevated cortisol levels have been linked to clinical and subclinical hypothyroidism.
Elevated cortisol also has an inverse relationship with testosterone. This means that the higher cortisol levels are, the lower the production of testosterone will be. Lower testosterone production then results in things like low libido, lower sperm production, and even lower energy.
Over time, lower testosterone levels are linked with a higher risk of developing metabolic diseases like diabetes, hypertension, hyperlipidemia, and cardiovascular problems.
In terms of reproduction in women, it is well known that chronic or high stress can cause irregular or absent menstrual cycles. Studies have shown that elevated cortisol decreases estradiol levels in the follicular phase of the menstrual cycles. This results in a delay in LH (luteinizing hormone) surges which stimulate ovulation. This impairs fertility and may even eliminate ovulation during this time.
Don’t let this worry you! Once the stressor is removed and cortisol levels return to normal, these effects have been shown to resolve.
Lastly, progesterone and estrogen interact with cortisol as well. These are the primary female sex hormones. Progesterone is also a precursor for the production of cortisol. Over time, chronic stress depletes our stores of progesterone and causes luteal phase deficiency. The luteal phase of the menstrual cycle is classified as the last 14 days, the time when most women experience PMS symptoms. Often times, hormonal balancing can help eliminate these problems altogether!
Having cortisol levels that are too high or too low can impact several functions in your body. The first step to remedying this situation is to know how to recognize a hormone imbalance related to cortisol in the first place.
If you experience chronic stress, cortisol levels will be elevated longterm. This is known as adrenal hyperactivity and is characterized by some or all of the following symptoms:
Over time, chronic stress will eventually push to the other end of the spectrum and lead to adrenal fatigue. This is also known as HPA axis dysregulation or adrenal insufficiency. This is when your adrenal glands are unable to keep up with your body’s demand for cortisol, causing levels to drop lower than the normal curve. This means having less cortisol to wake you up in the morning and keep you going throughout the day!
Think of your adrenal glands like a sponge. In the morning, you wake with a full sponge. As the day progresses and the brain signals for more cortisol, the sponge slowly squeezes it out until, by nighttime, your sponge has just a little left. Throughout the night, the sponge recharges and fully refills with cortisol.
In situations of chronic stress, the demand for cortisol throughout the day increases. This results in a completely drained sponge by the end of the day. As a result, the sponge does not refill completely overnight, causing you to begin the next day on an already low reserve of cortisol. This is what adrenal insufficiency looks like.
Once the body reaches this state, it readjusts and becomes used to it. If chronic stress continues, cortisol patterns will change again from a low pattern to a reverse cortisol pattern. Now that you are starting the day off with a half-full sponge, your reserve will deplete faster and cause a mid-afternoon drop in energy.
During this time, cortisol levels sink but the signals for cortisol continue. Once you fall asleep and your sponge begins to fill back up, cortisol will be secreted to satisfy the demand that was not met earlier. This spike in cortisol late at night is considered a reverse cortisol pattern and will commonly cause difficulty sleeping.
If you have some (or all) of the following symptoms, this may be happening with you:
If you read through either of the lists in this section and felt like you were looking at a list that perfectly describes you and your personal situation, it may be time to consult a doctor who can look at your levels and confirm whether your suspicions are true!
As you may suspect, there are also some diseases or disorders that could impact your cortisol levels. Being aware of these will make it much easier to understand possible links, especially if you already have a diagnosis!
Cushing’s Syndrome is a classic example of hypercortisolism. It is caused by either exogenous glucocorticoid medication (such as prednisone) or a cortisol secreting/stimulating tumor. This syndrome causes a defined set of symptoms seen in lesser intensities with subclinical adrenal hyperactivity, including:
Addison’s Disease is the primary cause of clinical hypocortisolism. This is caused by adrenal destruction, adrenal dysgenesis (improper formation of the adrenal glands during development), and impaired steroidogenesis (inability of the adrenal glands to produce cortisol). This disease results in:
In addition, other conditions (such as PCOS) can also correlate with cortisol imbalances. Ultimately, it’s worth asking your doctor if your symptoms could be related!
Finally, this brings us to the solutions you can look into if your cortisol levels are imbalanced. There are multiple ways you can regulate cortisol levels, so we’ll dive into each of them to give you a strong foundation.
Hydrocortisone: a prescription corticosteroid that acts in the body similarly to cortisol. Hydrocortisone should be taken in the morning before 10 a.m. to help replicate your natural surge of cortisol in the body. In low doses, it is used to treat moderate to severe hypocortisolism (adrenal fatigue) or HPA axis dysregulation.
Glandular Supplemental Support: classified as a supplement containing a desiccated adrenal gland. Glandular supplements come in a wide variety of options. Some contain only desiccated adrenal gland with varied doses while others contain additional herbal and nutrient support for optimal cortisol production. Consult with your naturopathic doctor to find the best supplement for your particular needs.
Also important to note, dessicated adrenal gland will act as a very low dose of cortisol in the system when taken orally. This should be taken in the morning before 10 a.m. when your cortisol is naturally at its highest. Glandular supplements are used to treat mild to moderate hypocortisolism, adrenal fatigue, and HPA axis dysregulation.
Many adrenal supplements contain an herbal and nutrient blend without containing adrenal glandulars for a more gentle approach to regulating the release of cortisol. These nutrients and herbs may also be found in glandular supplements to improve HPA regulation.
These supplements may be useful for both hypo and hypercortisolism. Herbal and nutrient adrenal supplements are generally used for mild cases of hypocortisolism/adrenalfatigue/HPA axis dysfunction. Plus, they are also used to prevent adrenal distress in times of chronic stress.
Adaptogens such as Astragalus, Ashwagandha, Rhodiola, and Ginseng have a balancing effect on cortisol production. They aid in both the treatment of hypo and hypercortisolism as well. These herbs also help reduce the impact of cortisol on the brain, resulting in neuroprotective properties.
Licorice root specifically helps with the treatment of hypocortisolism. This is due to a compound called glycyrrhizic acid which inhibits cortisol breakdown in the body.
Phosphatidylserine is an important component of the cell wall. It allows cell signalling that is vital to function. Supplementation helps to minimize the impact of acute and chronic stress on cortisol levels, so it is another important area to make sure you address.
Phosphatidylserine also acts at the level of the brain to decrease ACTH – the signal to release cortisol. Studies have shown that supplementation is particularly helpful in regulating cortisol in athletes to avoid negative side effects of over-training.
L-theanine is an amino acid known for its calming effects and enhancement of cognitive ability. L-theanine is shown to reduce stress response for one hour after supplementation, showing decreased levels of cortisol.
Magnesium, vitamin C, and zinc are also great supplements since they inhibit the production of cortisol in both chronic and acutely stressful situations.
Finally, pantothenic acid, or vitamin B5, is essential for proper production of coenzyme A and cortisol. Vitamin B5 deficiencies may lead to adrenal insufficiency.
Ultimately, I hope that you now understand just how important cortisol is when it comes to your body’s daily functions. Having balanced levels of cortisol is genuine crucial when it comes to living an energized, fulfilled life!
After today’s article, you should hopefully walk away with a solid understanding of:
Of course, if you have any other questions (whether they be about cortisol in general or your unique circumstances), don’t hesitate to reach out! What do you think could improve in your life from balancing your hormones?