By Dr. Roxanna Garcia, NMD / September 28, 2023

Did you know that approximately 23.5 million people are confirmed to be affected by autoimmune disease in the U.S.? But this number is actually suspected to be closer to 50 million, according to the American Autoimmune Related Diseases Association?
Could your symptoms be indicating an autoimmune disease?
In this article I will discuss the most common autoimmune diseases seen at Natural Med Doc.
Autoimmune diseases are a dysfunction of the immune system. Therefore, it is essential to understand how the immune system functions normally to understand autoimmune disease. For an in-depth explanation of the immune system and how it relates to autoimmune disease, check out What is Autoimmunity Article. However, I will give a brief overview here.
In autoimmune disease, our immune system, which normally helps protect us against harmful pathogens (such as bacteria and viruses) accidentally starts attacking our body’s own cells. This causes damage to our cells, inflammation, and eventually symptoms. We call this autoreactivity.
Now, everybody has some amount of autoreactivity in the body. But not everybody has an autoimmune disease. How does this happen?
Well, our immune system has an excellent memory and can make something called antibodies. Antibodies allow for the quick identification and destruction of pathogens we’ve come across in the past if we are re-exposed to the pathogen. This helps our immune system work more efficiently.
However with autoreactivity our immune system can make antibodies against our own cells, called autoantibodies. When autoantibodies identify our own body tissue, they will initiate an immune response and attack the tissue, causing damage, inflammation, and symptoms of autoimmune disease (which I will discuss in more detail below).
A significant factor in the production of autoantibodies and the development of an autoimmune disease is chronic inflammation.
Now, short-term inflammation is a helpful part of our healing process. Learn more about that by reading What is Autoimmunity.
Chronic inflammation will cause more tissue damage and actually creates an environment in which autoreactivity can occur more freely. This means that chronic inflammation not only exacerbates existing autoimmune diseases, but is also a contributing factor in developing autoimmune disease.
I will discuss more about triggers and risk factors in developing autoimmune disease in an upcoming article, so keep an eye out for that!
Now, conventional medicine describes autoimmune diseases as life-long conditions. At NMD, we work towards reversal and remission using diet, lifestyle, and other natural modalities.
What does that mean?
During the course of an autoimmune disease there can be periods of time where symptoms and disease activity are increased. These are called "flares.” In contrast, there are alternating periods of time when symptoms decrease or even disappear. We call this "remission."
This means you don't have to live with negative symptoms impacting your daily life!
Are you ready to learn more about the top 4 common autoimmune diseases we see at NMD?
Let's get started!

Rheumatoid arthritis (RA) is the most common chronic inflammatory joint disease, which affects the joints, cartilage, bone, and sometimes other parts of the body. [2] [6] [11]
If left untreated, RA can result not only in joint pain and damaged joints but also damage to the lung tissue, increased risk of cardiovascular disease, swelling and inflammation of the heart muscle, and increased risk of spinal injury. [11]
In fact, cardiovascular deaths are the cause of over half of the deaths in patients with RA. [9]
Even further, overall mortality (meaning the likelihood of death) is significantly higher for those with RA than the general population. And this is more pronounced in females with RA! [9]
This is why Rheumatoid arthritis absolutely must be addressed!
Risk factors:
There is a 2-3 times increased risk of developing RA for those with first-degree relatives who have an RA diagnosis, meaning there is a genetic component. [1]
However, the most important environmental and lifestyle risk factor for developing RA is current or past tobacco use. [1][2]
Notable dietary factors that increase risk for RA include Vitamin D deficiency, increased red meat consumption, excess coffee consumption, and high salt intake. [1]
What you may not know is the role that hormones play in RA progression. Our sex hormones, like estrogen and progesterone, are actually protective of our bones and joints when balanced appropriately. [11] During different life phases, when our hormone levels shift and potentially drift, inflammation can go unchecked. Examples include menopause phase of life, in cases of low testosterone, progesterone deficiency, and estrogen dominance. You now understand why that can be detrimental in autoimmune disease. The good news is that bioidentical hormone replacement is a natural and effective therapy which helps to balance these areas and ultimately target inflammation.
Another important factor in RA is the autoantibody called rheumatoid factor, or RF. Someone with RF-positive blood has a 26-fold increased risk of developing RA. This is because RF increases inflammation. [6] There we go again with inflammation!
For those who are already diagnosed with RA, we can use the RF levels in the blood to evaluate disease activity and therapy effectiveness, because RF levels fluctuate more so than the lab values. [6]
Signs and Symptoms: [5][8][10]
Rheumatoid arthritis is considered a systemic autoimmune disease, affecting many organ systems.
Common signs and symptoms seen in RA include:
Joints commonly affected include:
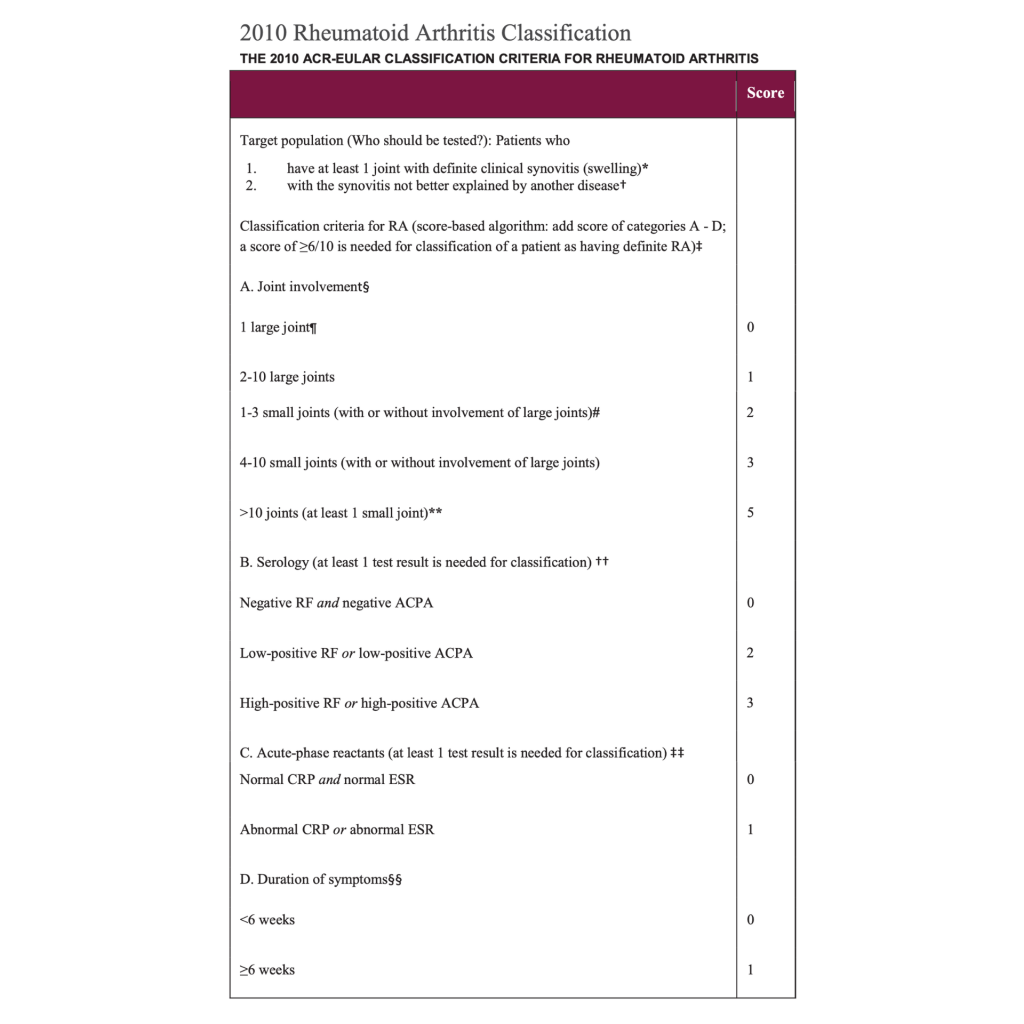
Diagnostic Criteria: [17] [18]
There is no specific test we can run to determine if someone has rheumatoid arthritis and this is true for most autoimmune diseases in general.
The way that rheumatoid arthritis is diagnosed is looking at criteria evaluating.
Generally, a score of 6 or more is classified as rheumatoid arthritis.
Prognosis:
Rheumatoid arthritis, like other autoimmune diseases, are considered life-long conditions for which there is no cure. [14]
It has also been observed that spontaneous remission, where signs and symptoms decrease or disappear without treatment, is uncommon, especially after the first 3-6 months of illness. [1]
This makes both early detection and early management of rheumatoid arthritis of extreme importance. If you have RA or suspect you may have RA, don’t delay and reach out today!
Even more alarmingly, many resources estimate that 40% of those diagnosed with RA will become disabled after 10 years. [13] [14]
This does not have to be the case for you or your loved ones!
We will treat the causes of your autoimmune disease, decrease inflammation, manage pain, and help with other symptoms.
But remember, we not only help manage pain or other symptoms, but improve overall health and quality of life. Our goal is to help you live your best life and having an RA diagnosis should not stop you from doing this!
If you are experiencing any of the symptoms discussed above, I recommend that you reach out to your naturopathic doctor today for proper evaluation and treatment options!
Systemic lupus erythematosus, or SLE, is a persistent inflammatory state that affects and damages multiple organs. Any organ can be affected, especially the skin, joints, kidneys, central nervous system, serous membranes, vessels, and the blood. [17]
About 90% of those with SLE are women with disease usually starting at reproductive age. [16] [17] [18]
Depending on the person, SLE can vary from slow-moving and relatively benign to rapidly progressive and potentially fatal. [12]
This is why we take SLE seriously!
Remember our chat about autoantibodies?
In patients with SLE over 100 autoantibodies have been recognized! [15]
There are a few we look at in particular, such as the antinuclear antibodies (ANA). [12]
Testing for ANA is the first step in determining if someone may have SLE, and in many cases, the types of autoantibodies present may result in different symptom presentations. [15]
This is why those with SLE can experience a wide range of symptoms, which we will discuss in the next section.
Signs and Symptoms:
SLE is considered a systemic autoimmune disease, meaning it can affect many organ systems and it often does. [15]
Symptoms may be chronic and persistent or relapsing-remitting, meaning they come and go. [18]
The most commonly affected organ systems are: [18]
Because symptoms vary from patient to patient, it is important to investigate a potential diagnosis of SLE for women of reproductive age if they have the “classic symptom triad” of fever, joint pain, and rash. [18]
Other signs and symptoms commonly seen in SLE include: [15] [18] [12]
As you can see, it can be difficult to determine if someone has SLE based on symptoms alone. Let’s discuss how SLE is diagnosed.
Diagnostic Criteria:
In 2019 there was an update for the criteria used to help diagnose SLE. This new criteria considers both lab values and symptoms.
The first step is to determine the presence of antinuclear antibodies (ANA). This is a blood test that a doctor orders and is not part of routine annual blood work. [18]
Once it has been determined that ANAs are present, different systems are looked at with a point-based system. Note: not all of these have to be present for a diagnosis.
A score of 10 or more is classified as SLE.
The signs and symptoms used for the diagnostic criteria include: [15] [16] [18] [19]

Prognosis:
The prognosis and severity of SLE is highly variable, even more so than for other autoimmune conditions. This is due to the wide variety of organ systems that can be affected. Overall, signs and symptoms tend to wax and wane throughout life.
Life expectancy for those with SLE has drastically improved over time. In fact, currently, the main cause of mortality in those with SLE is not due to the disease itself but rather from the side effects from medications, like immunosuppressants, or cardiovascular events. [20]
This is alarming! And this is why our naturopathic approach to treating SLE is not immunosuppression, but rather immune modulation. I will discuss more about conventional versus naturopathic treatment later in this article.
Furthermore, comorbidities of SLE have been linked to increased risk of mortality, and these include: infections, hypertension, lipid disorders, diabetes mellitus, bone-related conditions like osteoporosis, and some cancers. [20] A majority of these are areas of health that we work with at NMD! Meaning, not only do we work to improve symptoms of SLE, but we also address the associated comorbidities and reduce mortality.
It is important to investigate and manage SLE as soon as possible in order to prevent damage to all of these organ systems, improve symptoms, and live a healthier life!
Multiple Sclerosis (MS) is an organ-specific disease, affecting only the central nervous system (our brain and spinal cord). [22] It is a chronic progressive demyelinating disease of the central nervous system. [12]
That’s a lot of words, so let’s break it down!
If nerve cells are unable to transmit signals then any function of the body may be disrupted or unable to be carried out. For example if sensory nerve cells are not transmitting signals then your brain may not realize you are touching a hot pan, causing the injury to become worse due to the decreased response time.
Signs and Symptoms:
Because our brain and spinal cord control essentially all functions of the body, signs and symptoms can vary greatly depending on where the CNS is affected. [21][22]
Below are a list of common signs and symptoms in MS:
Additionally, MS is classified into 4 main types based on the way symptoms present: symptoms in MS can occur in different patterns. There are four main types: [21][25][12]
Clinically Isolated Syndrome (CIS) is really the beginning signs and symptoms of MS without meeting the criteria to be diagnosed as MS. CIS is the first event of symptoms that lasts 24 hours. The symptoms are neurological, such as numbness and tingling of limbs or even visual changes, and they occur as inflammation and demyelination begin to cause damage. [25] These changes occur in 85% of young adults who develop MS. However, the likelihood of developing MS after CIS varies and current prediciton methods are unreliable. It is estimated that 15-20 years after CIS, half of patients will develop secondary progressive MS, while a third of patients will have a bening course with minimal or no disability. [26]
In relapsing-remitting MS, symptoms present for about 4 weeks, then seem to completely (or partially) disappear, but return once again for another 4 weeks. Each time the cycle repeats, symptoms are at the same severity as before, meaning they have not worsened or progressed. This type of MS occurs in about 85% of those with the disease. [21][25] Also worth noting is that those with this type of MS tend to be diagnosed in their 20’s and 30’s on average, while the next two types are diagnosed during their 40’s and 50’s. [25]

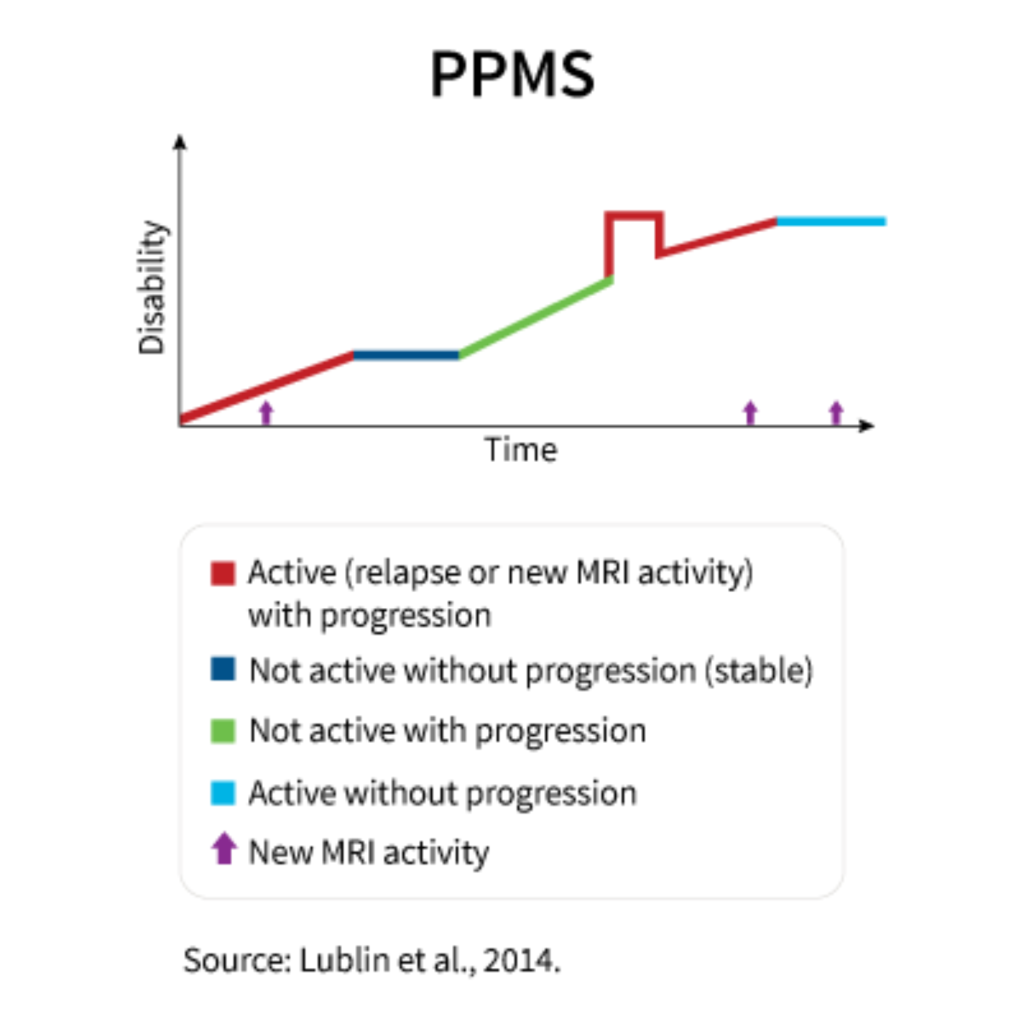
Primary progressive MS occurs in about 5-15% of cases. [21] Instead of the sudden-worsening, sudden-disappearing symptoms like the relapsing-remitting type, it is a gradual worsening of symptoms, especially those related to walking and movement. [25] Surprisingly, there is less inflammation and inflammatory cells seen with this type of MS, but this can make treatment and diagnosis more difficult. [25]
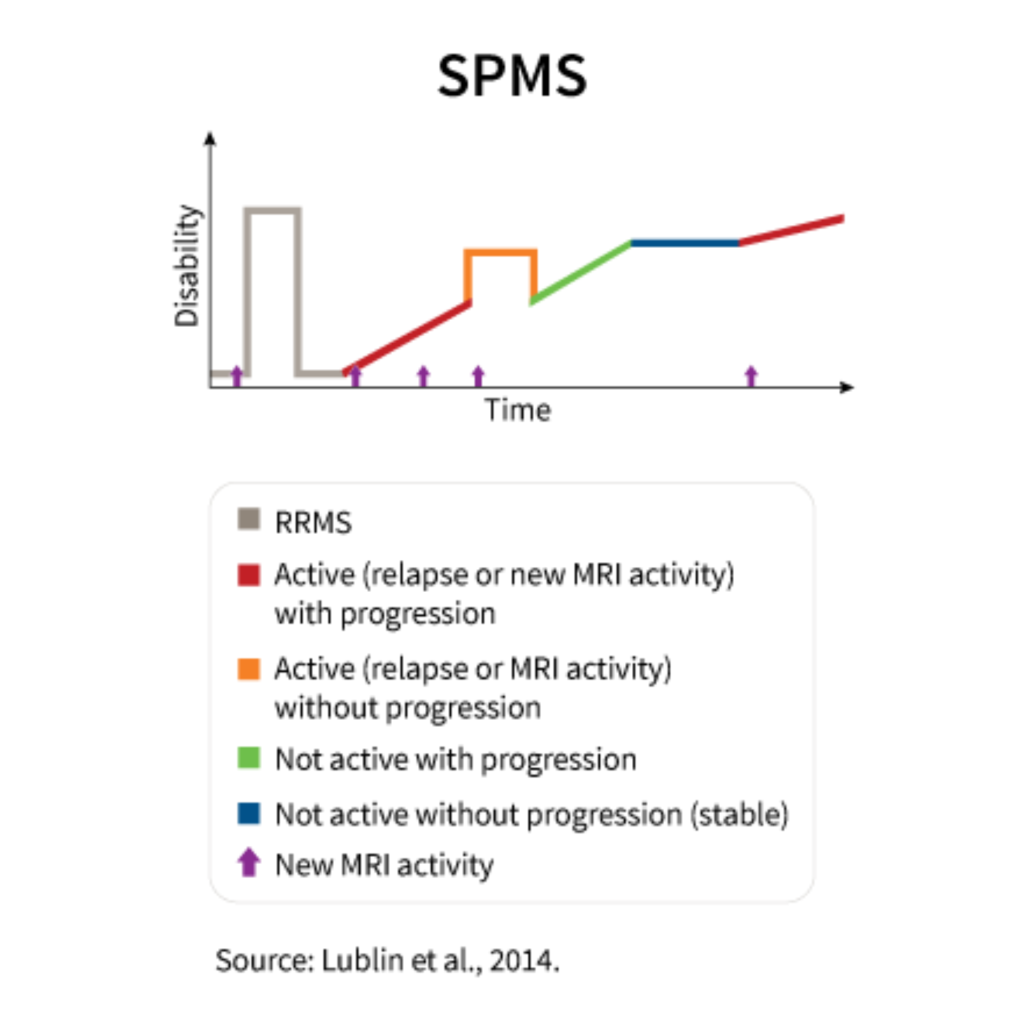
Secondary progressive MS usually occurs 10-25 years after the onset of relapsing-remitting MS. [24][25] It is the secondary phase of MS to explain the name. Here, symptoms switch from the relapsing-remitting cycle to gradually worsening over time without a noticeable transition between the two types. [24]
Diagnostic Criteria:
Like many other autoimmune diseases, there is no one test used to diagnose MS. In fact, MS can be difficult to obtain a diagnosis for because of the different symptom presentations, types of MS, and the diagnostic criteria itself. The diagnostic criteria for MS requires all three of the following: [25]
It goes without saying that those diagnosed with MS have gone through a long and difficult journey to obtain a diagnosis, while others are still working through that process. In either situation, we are here to support our patients!
Prognosis:
As far as prognosis, the main concern with MS is not necessarily a decreased lifespan, but rather is disability. Over 30% of those with MS will develop significant physical disability within 25 years of onset if left untreated. [27]
We don’t want this to happen to you!
If you have been diagnosed with MS or have any of the symptoms discussed above, please reach out today and get a proper assessment! There are ways that we can help manage symptoms and work towards remission.
Although not technically classified as an autoimmune disease currently, we include it here because fibromyalgia is inflammatory in nature and often accompanies many autoimmune diseases. [29]
Fibromyalgia is a long-term condition causing widespread body pain, low energy, poor sleep, brain fog, and other symptoms. [28]
It is unclear what causes fibromyalgia. [28] It is also unclear what happens in the body to cause the symptoms those with fibromyalgia experience, but it is suspected that it has something to do with the way the brain processes the sensation of pain. [28]
This does not mean it’s all in someone’s head! Fibromyalgia is a real condition and those who have it are experiencing real pain. This has been documented in research.
In fact, research shows that those who have fibromyalgia tend to have lower “pain thresholds.” This means that pain is experienced when only minimal pressure is applied to the body. In addition, pain intensity is experienced more strongly, meaning those with fibromyalgia will rate pain as more severe than those without fibromyalgia. [28]
This is why we take fibromyalgia seriously!
But fibromyalgia doesn’t only include feeling increased daily pain.
Let’s look at the other signs and symptoms of this condition.
Signs and Symptoms:
Common signs and symptoms include: [28][30][12]
Another important symptom of fibromyalgia is the presence of “tender points.” Tender points are areas on the body that are painful when pressed. These areas are usually in a muscle or tendon.
Diagnostic Criteria
Tender points used to be a part of the diagnostic criteria, but in 2010 they were excluded. Updated criteria now looks at a few different things.
Diagnosis of fibromyalgia is when these three conditions are met: [28]
Overall, it can be difficult to diagnose fibromyalgia because many of the symptoms overlap with other conditions and because the diagnostic criteria requires these other conditions be investigated, designating fibromyalgia as a diagnosis of exclusion.
Unfortunately, by the time they visit us, many of our patients have been to multiple doctors, have had multiple tests run with results that come back “normal,” but still do not have an answer or satisfactory treatment plan to address their pain. We want to manage your pain, optimize your health, and help you get to where you want to be!
Prognosis:
Fibromyalgia is described as a “chronic relapsing condition,” meaning that symptoms will continually come and go over a long period of time. [31] It is also considered not life-threatening, non-deformative, and non-progressive. However, we know that fibromyalgia can considerably affect your quality of life, even if it’s not causing joint deformities.
Furthermore, did you know that fibromyalgia, specifically low energy, chronic pain and chronic inflammation, can increase risk of metabolic syndrome, such as diabetes? [31]
At NMD we consider the body as a whole and focus on helping prevent the development of conditions like diabetes, as well as helping to manage symptoms of fibromyalgia.

With conventional medicine treatments tend to be generalized for all autoimmune diseases. Most treatments focus on anti-inflammatory and/or immunosuppressive agents. This includes over-the-counter pain medications (NSAIDs, aspirin, ibuprofen, naproxen, tylenol/acetaminophen), corticosteroids (prednisone, cortisone shots), and methotrexate. These can be helpful tools, especially during severe flares when symptoms are worse; however, these medications tend to have major side effects and may not be best for long term management of autoimmune diseases.
Naturopathic medicine addresses chronic inflammation and immune dysfunction (such as autoreactivity, autoantibodies, and tissue damage resulting in symptoms). There are many ways these factors can be addressed. Specifically, we prefer immune modulation over immunosuppression, meaning we help to balance the immune system rather than stifle it. Examples of naturopathic approaches include dietary recommendations, nutrients, botanicals, gut healing protocols, hormone balance, and so much more!
Treatment must be individualized because no two people are the same, even if they have the same autoimmune disease. We recognize this and use what works best for your body, specifically. For more details about naturopathic treatment, keep an eye out for Autoimmunity Mega Article.
In this article we learned about the top autoimmune conditions seen at Natural Med Doc. We discussed the most common symptoms, diagnostic criteria, and prognosis for each of these.
Obtaining a diagnosis for your symptoms can be a long and difficult journey with autoimmune disease, but we are here to investigate and help with this!
Plus, we will support the body by managing inflammation, modulating the immune system, and working towards remission.
Our goal is to help you live your best life and having an autoimmune disease should not stop you from doing this!